When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But what if the batch of generic medicine you’re holding was made from a different recipe than the one tested in the lab? That’s not a hypothetical. It’s a real problem hiding in plain sight - and it’s called batch variability.
What Is Batch Variability, and Why Should You Care?
Every drug batch - whether it’s the brand-name version or a generic - is made in a factory, not in a perfect, repeatable machine. Even with strict controls, tiny differences in mixing time, temperature, or raw material purity can change how the drug behaves in your body. These differences show up in pharmacokinetic (PK) data: how fast the drug enters your bloodstream, how high the peak concentration gets, and how long it stays there. For years, regulators assumed these differences were small enough to ignore. But a 2016 study in Clinical Pharmacology & Therapeutics found something startling: between-batch variability accounts for 40% to 70% of the total error in bioequivalence studies. That means if you test just one batch of a generic drug against one batch of the brand, you’re not really testing the drug - you’re testing two specific batches. And if those batches happen to be unusually similar or different, the whole conclusion could be wrong.The 80-125% Rule: A Flawed Benchmark
The current gold standard for proving bioequivalence is the 80-125% confidence interval for the ratio of key PK values - AUC (total exposure) and Cmax (peak concentration). If the test drug’s values fall within that range compared to the reference, it’s declared bioequivalent. This rule was set by the FDA in 1992 and later adopted worldwide. But here’s the catch: this rule doesn’t care where the variability comes from. It treats all noise the same. If the brand-name drug itself has inconsistent batches - say, one batch delivers 110% of the expected dose and another delivers 90% - the test drug only needs to match the *specific batch* used in the study. It doesn’t need to match the *typical* performance of the brand. This creates a dangerous loophole. A generic drug could be approved based on a lucky match with a low-variance reference batch, even if it would fail against other batches of the same brand. Or worse - a perfectly good generic could be rejected because it was tested against an unusually variable reference batch.Why Single-Batch Testing Isn’t Enough
Right now, the rules require the test product to come from a batch that’s at least 1/10th of full production scale - or 100,000 units, whichever is bigger. The reference batch must be representative, but there’s no requirement to test multiple batches of the reference product. A 2016 controlled study showed what happens when you test the same brand-name drug across multiple batches. The point estimates for bioequivalence shifted dramatically - sometimes crossing the 80-125% line just by switching batches. That’s not a flaw in the generic. That’s a flaw in the test design. Imagine testing two cars for fuel efficiency, but only using one car from each manufacturer - and one of those cars happened to have a faulty fuel injector. Would you say the whole model line is inefficient? No. But that’s exactly what happens in bioequivalence testing today.
The New Approach: Between-Batch Bioequivalence (BBE)
A better way is emerging: Between-Batch Bioequivalence, or BBE. Proposed in 2020 and backed by real-world simulations, BBE doesn’t just compare the test drug to one reference batch. It compares it to the *natural variability* of the reference product itself. Here’s how it works: First, you test at least three batches of the brand-name drug. You measure how much they vary from each other - say, the standard deviation in Cmax is 12%. Then, you test the generic against those same batches. If the average difference between the generic and the reference is less than twice that standard deviation (in this case, less than 24%), the generic passes. This approach doesn’t require bigger studies or more patients. It just requires smarter math. And it’s already being used for tricky products like nasal sprays and inhalers, where tiny manufacturing changes can have big effects. The FDA’s 2022 guidance on budesonide nasal spray quietly adopted this logic. It asked for “super-batch variability” - pooling all batches to understand true product variation. That’s a big step. But it’s still an exception, not the rule.What Experts Are Saying
Dr. Robert Lionberger, former head of the FDA’s Office of Generic Drugs, called ignoring batch variability “one of the most significant statistical oversights in modern bioequivalence.” He warned it leads to both false approvals and false rejections. Dr. Donald Schuirmann, a leading biostatistician, showed that under high batch variability, the error rate in bioequivalence studies can exceed the accepted 5% threshold - meaning you’re more likely to get the wrong answer than you think. The European Federation for Pharmaceutical Sciences (EUFEPS) issued a 2021 call for regulatory action, saying: “Current guidelines are inadequate for complex products.” And the EMA’s 2023 workshop on complex generics listed “inadequate consideration of batch-to-batch variability” as one of the top three challenges in generic drug approval.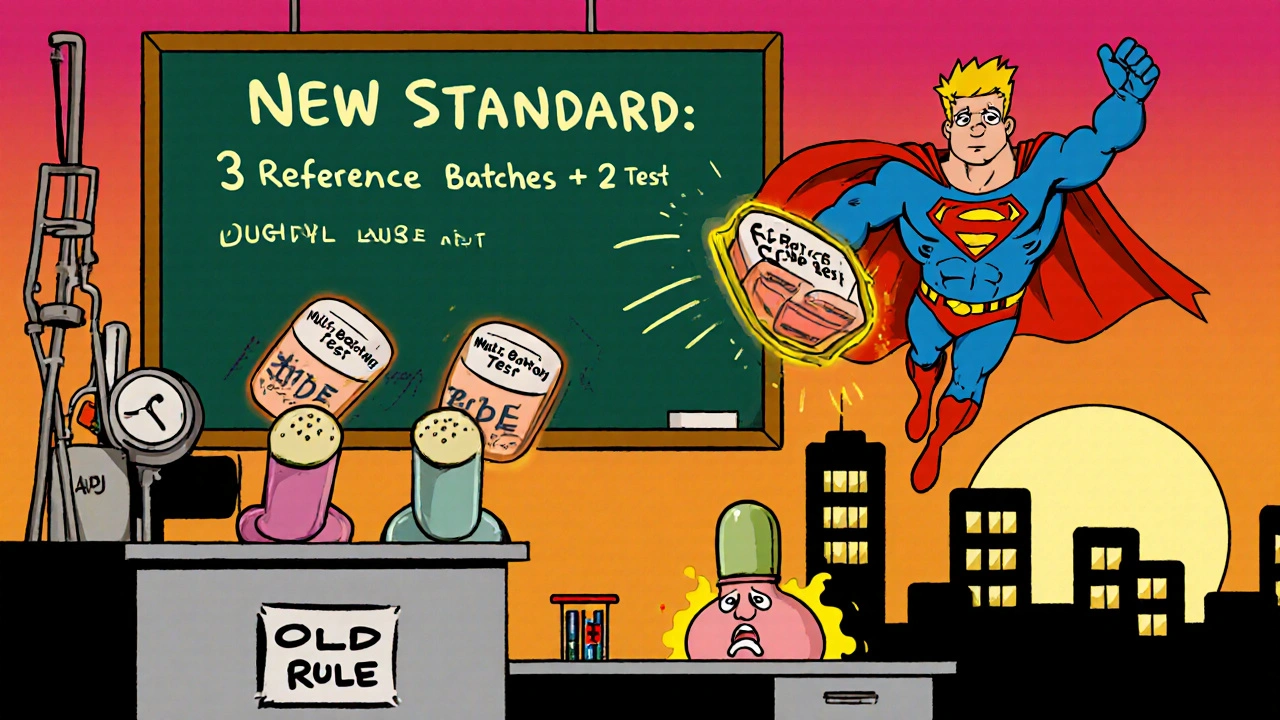
What’s Changing - and When
The industry is catching up. In 2018, only 32% of major generic manufacturers tested multiple batches. By 2022, that number jumped to 78%. Why? Because regulators are starting to demand it. The FDA’s draft guidance from June 2023, titled “Consideration of Batch-to-Batch Variability in Bioequivalence Studies,” proposes making multi-batch testing mandatory for certain products. Final guidance is expected in early 2024. The EMA is also reviewing its guidelines and plans public consultation in late 2023. By 2025, experts predict the standard will shift. You’ll need at least three reference batches and two test batches. The statistical model will separate within-subject error from between-batch error. And the 80-125% rule? It won’t disappear - but it will be used alongside new, smarter criteria.What This Means for Patients and Prescribers
You don’t need to understand mixed-effects models or standard deviations to benefit from this change. But you should know this: the system is finally waking up to a problem that’s been hiding for decades. Better batch testing means fewer bad generics slipping through. It also means fewer good generics getting unfairly rejected. That’s good for patients who rely on affordable medication - and for doctors who need to trust that a generic will work just like the brand. The bottom line? Bioequivalence isn’t just about numbers on a chart. It’s about real people getting the right dose, every time. And that only happens when the system accounts for the messy reality of manufacturing - not just the ideal version of it.What You Can Expect in the Near Future
- Generic drug applications will require data from multiple production batches - not just one. - Regulatory submissions will include variance decomposition: separating batch-to-batch differences from patient-to-patient differences. - For complex products like inhalers, nasal sprays, and topical gels, multi-batch testing will become standard - not optional. - The 80-125% rule will still be used, but it won’t be the only criterion. - You’ll see more transparency: manufacturers will publish batch characterization data, not just summary results. This isn’t about making generic drugs harder to approve. It’s about making sure the ones that *are* approved actually work the way they’re supposed to - no matter which batch you get.What is batch variability in generic drugs?
Batch variability refers to small but meaningful differences in how a drug performs between different production runs. Even if two batches of the same drug are made to the same formula, factors like mixing time, ingredient purity, or temperature can cause slight changes in how quickly the drug enters the bloodstream or how much of it gets absorbed. These differences can affect whether a generic drug is truly equivalent to the brand-name version.
Why does batch variability matter for bioequivalence?
Current bioequivalence tests compare just one batch of the generic to one batch of the brand. If those two batches happen to be unusually similar, the test may falsely show equivalence. If they’re unusually different, a good generic might be wrongly rejected. Since batch variability can make up 40-70% of the total error in studies, ignoring it risks approving ineffective drugs or blocking effective ones.
Is the 80-125% bioequivalence rule still valid?
Yes - but it’s incomplete. The 80-125% confidence interval for AUC and Cmax remains the legal standard for approval. However, new guidance from the FDA and EMA now recommends supplementing this with multi-batch testing and statistical models that account for between-batch variation. The rule isn’t being scrapped - it’s being upgraded.
Which drug products are most affected by batch variability?
Products with complex delivery systems are most sensitive. This includes nasal sprays, inhalers, topical creams, and injectables - where tiny changes in particle size, viscosity, or formulation can drastically alter how the drug is absorbed. Even some oral solids with low solubility (like certain antifungals or antivirals) show high batch-to-batch variation in absorption.
What is Between-Batch Bioequivalence (BBE)?
BBE is a new method that compares the average performance of a generic drug to the natural variability of the brand-name product across multiple batches. Instead of requiring the generic to match a single reference batch, BBE checks whether the generic’s average performance falls within the range of the brand’s own batch differences. This makes the test more realistic and less prone to false results.
Will this change make generic drugs more expensive?
Not significantly. While testing multiple batches adds cost, it’s a one-time investment for manufacturers. The real savings come from reducing failed approvals and costly recalls. Most major generic companies already test multiple batches for complex products - the change just makes it mandatory. Patients will still get affordable options - just more reliable ones.
When will these new standards take effect?
The FDA’s final guidance is expected in early 2024. The EMA is reviewing its guidelines with public consultation planned for late 2023. By 2025, multi-batch testing with variance analysis will be required for complex generics like inhalers and nasal sprays. For simpler oral tablets, the transition may take longer, but the trend is clear: the old single-batch model is being phased out.