Heat Safety Hydration Calculator
Your Heat Safety Hydration Calculator
This calculator estimates your recommended daily fluid intake based on your medications, temperature, and activity level.
Your Recommended Fluid Intake
Based on CDC guidelines for diuretic and anticholinergic users during heat events
Heat Safety Tip
For every 10°F above 80°F, increase fluid intake by 0.5 liters (about 16 oz) when on diuretics or anticholinergics.
When the temperature climbs, people on certain meds face a hidden danger that most of us don’t think about. Diuretics are blood‑pressure and heart‑failure pills that make you pee more, while Anticholinergics are drugs for bladder control, depression, and allergies that blunt the body’s ability to sweat. Both groups can turn a hot day into a medical emergency if you don’t take extra precautions. This guide explains why, what the science says, and exactly what you can do to stay safe.
Why Diuretics Make Heat Riskier
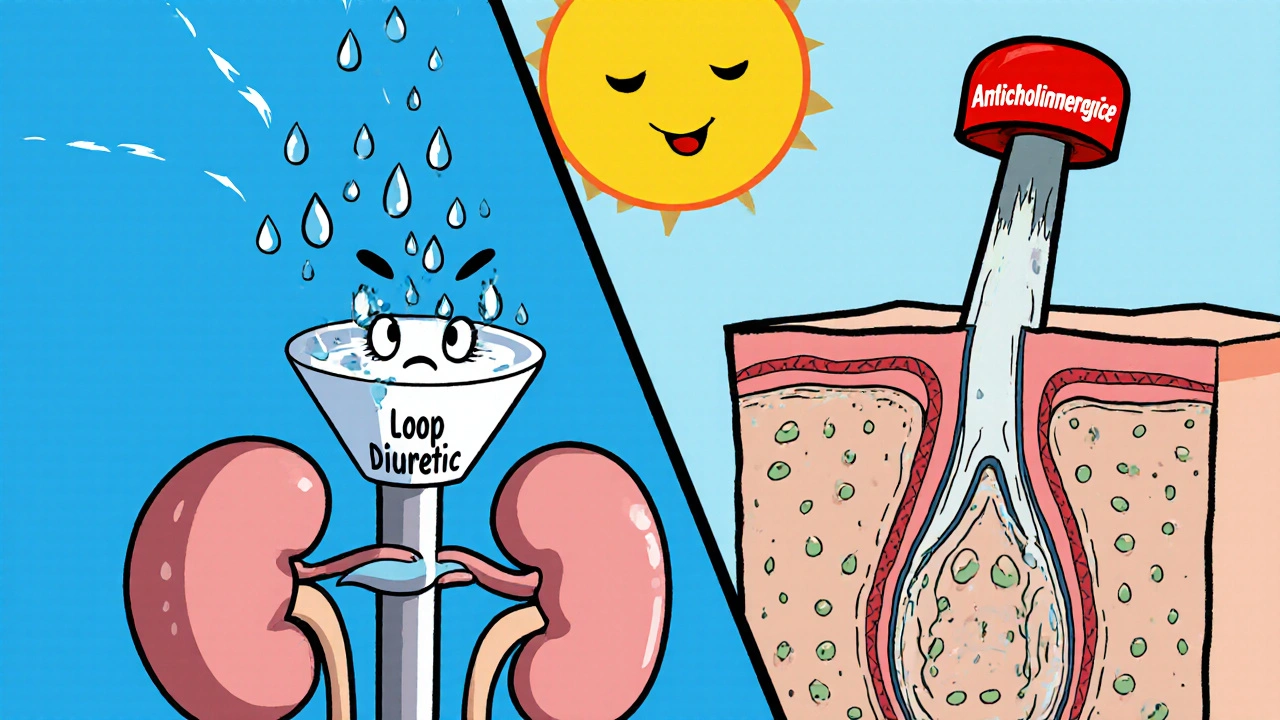
Diuretics work by pushing sodium and water out of the kidneys. Loop agents like furosemide (Lasix) hit the thick ascending limb of the loop of Henle, while thiazides such as hydrochlorothiazide act farther down the tubule. The result is a lower plasma volume and, in many cases, loss of potassium.
When you’re sweating 1-2 liters per hour in extreme heat, that fluid‑saving capacity is priceless. Lose it, and core temperature spikes faster, heart rate climbs, and you become prone to heat cramps, syncope, or even heat stroke. A 2022 study of 1.2 million Medicare beneficiaries showed loop‑diuretic users had a 37 % higher risk of heat‑related hospitalization compared with non‑users, even at temperatures as low as 80 °F (26.7 °C).
How Anticholinergics Block Your Body’s Cooling System
Anticholinergic drugs block muscarinic receptors, which are essential for activating sweat glands. High‑burden agents-those with an Anticholinergic Cognitive Burden (ACB) score of 3-include oxybutynin (Ditropan), tolterodine (Detrol), and tricyclic antidepressants like amitriptyline (Elavil). Laboratory work in the Journal of Thermal Biology found these drugs cut sweat output by 30‑50 %.
Without sweat, the body can’t evaporate heat. In the 2021 Pacific Northwest heat dome, 91 % of the 800+ heat‑related deaths involved at least one medication affecting thermoregulation, and diuretics or anticholinergics were present in 63 % of those cases. For older adults, the problem is amplified: reduced baseline sweat rates, cognitive changes, and polypharmacy all converge.
Official Guidance from Public Health Agencies
The Centers for Disease Control and Prevention (CDC) lists diuretics and anticholinergics among the top medication classes that demand extra vigilance during heat waves. Their 2023 Heat and Medications Guidance advises clinicians to:
- Consider temporary relaxation of fluid‑restriction orders for patients on diuretics during extreme heat.
- Identify a "point of contact"-a family member, friend, or caregiver-who can check on the patient at least twice daily.
- Educate patients about early symptoms of heat‑related illness (dizziness, rapid pulse, confusion).
Houston Methodist’s Dr. Shah adds practical tips: drink water regularly, seek shade, wear loose, light‑colored clothing, and apply broad‑spectrum sunscreen (many anticholinergics increase photosensitivity).
Practical Precautions You Can Start Today
Below is a checklist you can keep on your fridge or phone.
- Hydration plan: Aim for at least 2 L of water daily on hot days, unless your doctor has set a strict limit for heart‑failure fluid balance. Sip, don’t gulp.
- Electrolyte monitoring: If you’re on a thiazide, test potassium weekly during summer. Low potassium can cause muscle weakness and cardiac arrhythmia.
- Clothing strategy: Choose breathable fabrics (cotton, linen) and light colors. A loose hat protects against sun‑induced dehydration.
- Cooling devices: Portable fans, cooling towels, or a simple bowl of ice water for hand immersion can offset reduced sweat.
- Buddy system: Have someone call or visit you twice a day during heat alerts. They can spot early signs of confusion or lethargy.
- Medication review: Ask your prescriber if dose reduction or a switch to a lower‑burden agent is safe for the heat season.
Medication Management Strategies
Clinicians have a few evidence‑based levers:
- Temporary dose adjustment: A pilot at Massachusetts General Hospital showed 42 % of heart‑failure patients needed a short‑term reduction in loop‑diuretic dose during a July 2022 heatwave.
- Switching agents: For patients on high‑burden anticholinergics, consider alternatives with ACB ≤ 2 (e.g., solifenacin instead of oxybutynin) when the risk outweighs the benefit.
- Scheduled laboratory checks: Serum sodium, potassium, and creatinine every 2-4 weeks in summer for patients on combined diuretic‑anticholinergic regimens.
Never stop a prescribed medication without a doctor’s order-abrupt withdrawal can trigger rebound hypertension, heart‑failure decompensation, or worsening urinary symptoms.
Evidence Gaps and Ongoing Research
While the association between these drug classes and heat illness is clear, causality is still being ironed out. Dr. Lisa Pasternack (Johns Hopkins) notes most data come from case reports and small observational studies. To fill the gap, the National Institute on Aging funded a $4.2 M program in 2024 focused on thermoregulation in older adults taking diuretics and anticholinergics. Penn State’s Dr. W. Larry Kenney leads a $2.8 M NIH‑funded trial (R01AG077821) that will report preliminary findings in Q2 2025.
In the meantime, the CDC’s Heat and Health Tracking System is integrating medication‑use data to build predictive risk models. As climate change pushes the number of >90 °F days up by nearly 50 % since 1970 (NOAA), clinicians and patients must act on the best available guidance.

Quick Reference Table
| Aspect | Diuretics | Anticholinergics |
|---|---|---|
| Primary mechanism affecting heat tolerance | Fluid loss → reduced plasma volume | Sweat inhibition → impaired evaporative cooling |
| Common high‑risk agents | Furosemide, Hydrochlorothiazide, Chlorthalidone | Oxybutynin, Tolterodine, Amitriptyline |
| Electrolyte impact | Risk of hyponatremia, hypokalemia | Generally neutral, but may cause dry mouth |
| Typical heat‑related symptom onset | Dehydration, dizziness, rapid heart rate | Dry skin, low sweat, early confusion |
| CDC precaution flag | Adjust fluid restrictions during heat alerts | Identify caregiver check‑in; consider dose review |
| Evidence strength (2023‑2024) | Observational data, 37 % higher hospitalization risk | Experimental reductions in sweat 30‑50 % |
Bottom Line Checklist
- Know whether you’re on a diuretic, an anticholinergic, or both.
- Keep a water bottle handy; aim for at least 2 L on hot days (adjust if your doctor says otherwise).
- Check electrolytes if you’re on a thiazide diuretic.
- Dress in light, breathable fabrics and use a cool hat.
- Set up a buddy system for daily check‑ins during heat warnings.
- Talk to your clinician about temporary dose changes before the heat season starts.
- Stay aware of early heat‑illness signs: dizziness, rapid pulse, confusion, reduced urine output.
- Never stop medication without medical guidance.
Frequently Asked Questions
Can I take an over‑the‑counter pain reliever while on diuretics in hot weather?
Yes, but choose acetaminophen over NSAIDs. NSAIDs can reduce kidney blood flow and worsen the fluid‑loss effect of diuretics, increasing the risk of acute kidney injury in the heat.
If I’m on a low‑dose thiazide, do I still need extra water on a 85 °F day?
Absolutely. Even modest temperatures trigger insensible losses through respiration and skin. A daily intake of 1.5-2 L is a good baseline, unless your cardiologist has set a stricter limit.
My anticholinergic prescription says to avoid alcohol. Does that also apply to staying hydrated with sports drinks?
Alcohol is the concern because it further dehydrates you. Sports drinks that contain electrolytes are fine, especially if they help replace sodium and potassium lost through sweat.
Should I stop my diuretic during a heat wave if I feel fine?
Never stop a prescription on your own. Contact your prescriber - they may suggest a temporary dose reduction, but abrupt discontinuation can cause blood‑pressure spikes or fluid overload.
What are the early signs that my medication is making me heat‑intolerant?
Watch for dizziness, excessive thirst, dark urine, rapid heartbeat, confusion, or a sudden drop in urine output. If any appear, seek medical attention promptly.