Managing medications at home isn’t just about remembering to take pills. It’s about safety, timing, interactions, and knowing what to do when something goes wrong. For older adults or anyone with chronic conditions, the burden often falls on family members or unpaid caregivers. And it’s not just a nice thing to do-it’s a medical necessity. Nearly half of all medication errors happen at home, and medication non-adherence causes over 125,000 preventable deaths in the U.S. every year. The good news? Getting family or caregivers involved the right way can cut those risks dramatically.
Start with a Complete Medication List
Before you do anything else, write down every medication the person takes. Not just the name-every detail matters. That means brand name, generic name, dosage (like “Lisinopril 10mg”), how often it’s taken (e.g., “once daily at 8 AM”), and whether it should be taken with food. Include the prescribing doctor’s name and phone number, the reason for the medication, and any known side effects or interactions. The Agency for Healthcare Research and Quality says a full list should have 17 data points per medication. Most people only list 3 or 4. That’s not enough.Update this list within 24 hours of any change-whether it’s a new prescription, a dose adjustment, or a drug being stopped. Hospital discharges are the most dangerous time. Studies show 50-60% of medication errors happen when someone comes home from the hospital. Bring the list to every doctor’s visit. One caregiver in Ohio told her story on the Caregiver Action Network forum: “I caught a dangerous interaction between my mom’s blood pressure med and her arthritis drug because I had the full list. The pharmacist said if I hadn’t brought it, she could’ve ended up in the ER.”
Use Tools That Actually Work
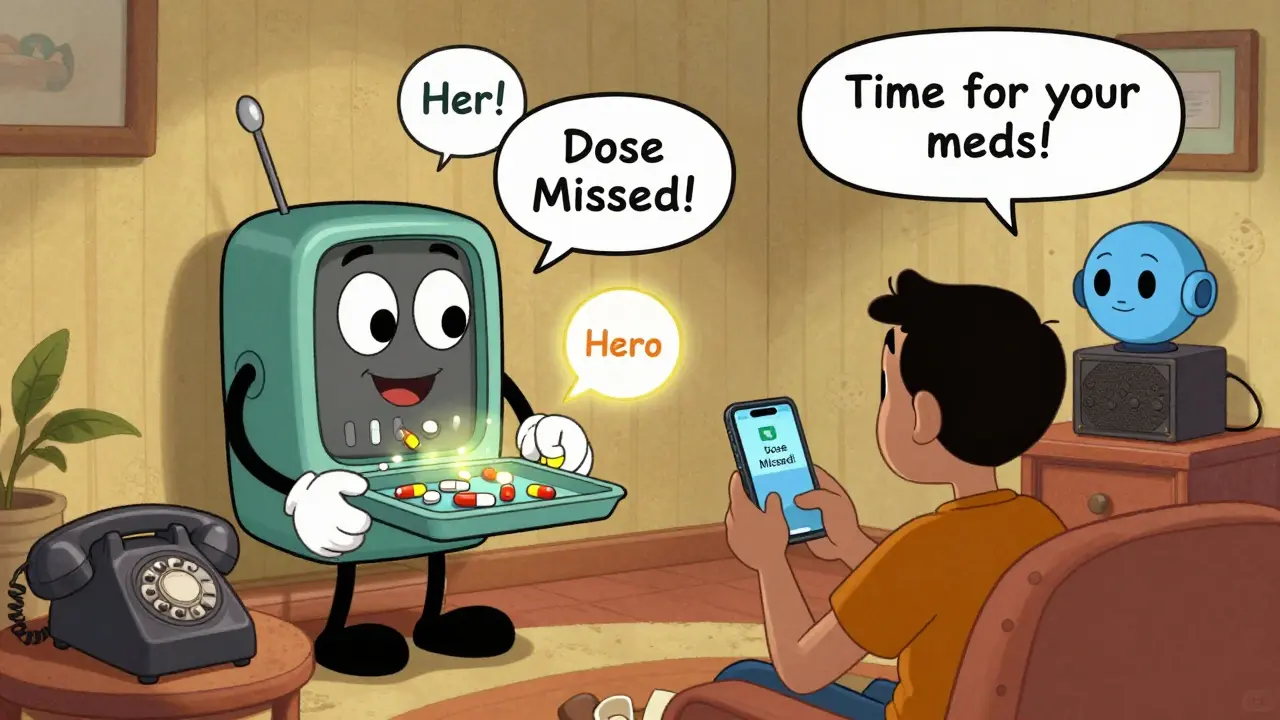
Paper reminders? They get lost. Mental notes? They fail under stress. Reliable systems exist-and they’re proven.Simple 7-day pill organizers with morning and evening compartments reduce missed doses by 37%, according to the Journal of the American Geriatrics Society. For more complex regimens, electronic dispensers like Hero Health or MedMinder automatically release pills and send alerts to phones. Clinical trials show these devices cut missed doses by 62%. If the person uses Alexa or Google Home, set up voice reminders. A University of Pittsburgh study found voice alerts reduced missed doses by 37% for people with memory issues.
Apps like Medisafe or Round Health send push notifications, track adherence, and can even alert family members if a dose is skipped. Users report 45% better adherence compared to paper logs. Don’t just rely on the phone’s alarm clock. Those get silenced. Use a dedicated tool built for this.
Build Routines, Not Reminders
The brain remembers habits better than alarms. Link medication times to daily routines you already do. This is called “habit stacking.” Take blood pressure pills right after brushing your teeth. Take diabetes meds before lunch. Take evening painkillers after dinner. The National Institute on Aging says this technique increases adherence by 28%.Don’t try to create a whole new schedule. Attach the medication to something already ingrained. If the person eats breakfast at 8 a.m., that’s the time for morning meds. If they watch the news at 6 p.m., that’s when the evening ones go in. Consistency beats complexity.
Know When to Ask the Pharmacist
Pharmacists are the most accessible medication experts in the healthcare system. Ninety-two percent of U.S. pharmacies have pharmacists on-site without an appointment. Don’t wait for a doctor’s visit. Walk in with your medication list and ask four key questions:- What time should this be taken relative to meals?
- Are there foods, drinks, or other meds it shouldn’t be taken with?
- What should I do if a dose is missed?
- When should I expect to see results?
Ask about the Beers Criteria. It’s a list of 30 medications that are risky for older adults. If someone’s on 5 or more drugs (which 45% of seniors are), ask if any of them are on this list. Many doctors don’t check unless prompted. A 2023 Medscape article warned that polypharmacy increases fall risk by 50% and hospitalization risk by 30%. You need to be the one asking.
Set Up Automatic Refills
Running out of meds is one of the top reasons people miss doses. Most major pharmacies-CVS, Walgreens, and others-offer free automatic refills through Medicare Part D or private insurance. Sign up for it. Set it to refill 7-10 days before the prescription runs out. You’ll get a text or email when it’s ready. No more scrambling.Some pharmacies now offer delivery or curbside pickup. If the person can’t leave the house, this is a game-changer. Walgreens launched its Caregiver Support Hub in March 2024. CVS Health now integrates in-home medication reviews through its Signify Health acquisition. These services exist. Use them.
Do Quarterly Medication Reviews
Medications change. Conditions change. What worked six months ago might be unnecessary-or dangerous-now. The American Geriatrics Society recommends a full medication review every three months for anyone taking four or more drugs. Bring the updated list to the doctor. Ask: “Is every pill still needed?” “Can any be stopped?” “Are there cheaper or safer alternatives?”Studies show that regular reviews reduce inappropriate prescriptions by 22%. One caregiver in Michigan told her story on Reddit: “I brought the list to every specialist. Nobody knew what the others prescribed. After I showed them the full picture, my dad had three drugs taken off his list. He felt better immediately.”
Prepare for Emergencies
Not all missed doses are equal. Some meds, like insulin, blood thinners, or heart medications, can cause life-threatening problems if skipped. Create a “medication red list.” Write down which drugs require immediate medical attention if missed. Tape it to the fridge. Give copies to all caregivers. Include contact numbers for the doctor and poison control.Annals of Internal Medicine found that families who used a red list reduced emergency room visits by 19%. It’s not about fear-it’s about readiness. When the power goes out and the electronic dispenser stops working, you need to know what to do next.

Attend Appointments Together
Doctors don’t always ask the right questions. They’re rushed. They assume the patient remembers everything. Go to every appointment with the person you’re helping. Take notes. Ask questions. Bring the medication list. A 2023 AARP survey found that 89% of caregivers who attended appointments reported better understanding of the medication plan. That’s the difference between confusion and control.Bring up side effects. Ask about cost. Say, “We’re struggling to keep up with this schedule.” The doctor can’t help if they don’t know there’s a problem.
Watch for Burnout
Medication management is exhausting. The National Alliance for Caregiving found that 42% of caregivers say managing meds is their most stressful task. You’re not failing if you’re overwhelmed. It’s a heavy job.Look for help. Talk to the doctor about Medication Therapy Management (MTM) services. Medicare Part D requires these for people taking 8+ drugs with 3+ chronic conditions. In 2023, 68% of eligible beneficiaries used them. Private insurers offer them too. A pharmacist reviews all meds, checks for interactions, and simplifies the plan. It’s free if you’re on Medicare Part D.
Don’t try to do it alone. Ask other family members to share the load. Hire a home care aide for medication assistance if possible. Use community resources. The goal isn’t perfection-it’s sustainability.
What’s Next?
Technology is getting smarter. The FDA has approved 12 digital pill systems since 2017. AI assistants like Alexa Care Hub saw 200% growth in 2023. By 2027, 65% of caregiver medication support will likely involve AI tools. But the foundation won’t change: clear lists, routine habits, pharmacist input, and shared responsibility.Right now, 59.4 million Americans are over 65. Eighty-two percent take two or more prescriptions. Forty-five percent take five or more. The system is overloaded. But families can fill the gaps-if they have the right tools and support.
You don’t need to be a nurse. You just need to be organized, persistent, and willing to ask questions. Start with the list. Use a pill organizer. Talk to the pharmacist. Set up automatic refills. Do a quarterly review. And remember: you’re not just helping someone take pills. You’re helping them stay safe, stay healthy, and stay home.
Can I just use a pill organizer instead of talking to a pharmacist?
A pill organizer helps with timing, but it doesn’t check for dangerous interactions, side effects, or unnecessary medications. Pharmacists catch errors that organizers can’t. For example, a person might be taking two drugs that both cause dizziness. The organizer will still dispense both. The pharmacist will flag the risk. Use both together.
What if the person refuses help with their meds?
Respect their autonomy, but don’t give up. Start small. Say, “I’m just going to help you refill your pills this month.” Or, “Can I sit with you while you take your morning meds?” Build trust. Show up consistently. Often, resistance comes from fear of losing control. Frame help as partnership, not takeover. If safety is at risk, talk to the doctor. They can explain why support is medically necessary.
Are there free tools for caregivers?
Yes. Medicare Part D offers free Medication Therapy Management (MTM) for eligible patients. Most pharmacies provide free automatic refills and pill organizers. Apps like Medisafe have free versions with basic reminders. The Caregiver Action Network offers a free printable Medication Tracker. Local Area Agencies on Aging often provide free caregiver coaching. You don’t need to spend money to get support.
How do I handle meds when traveling?
Keep meds in their original bottles with labels. Carry a copy of the medication list. Use a small pill organizer for daily doses. If flying, pack meds in your carry-on. Never check them. Set phone alarms for time zone changes. If the person takes insulin or other temperature-sensitive drugs, bring a cooler. Always have extra doses in case of delays.
What should I do if a dose is missed?
Don’t guess. Check the medication guide or call the pharmacist. For most meds, if you miss a dose and it’s within a few hours, take it then. If it’s almost time for the next dose, skip the missed one. Never double up unless instructed. For critical meds like blood thinners or insulin, call the doctor immediately. Have a red list ready so you know which situations require urgent action.
How often should the medication list be updated?
Update it within 24 hours of any change: new prescription, dose change, or drug stopped. Also update it after every hospital visit, ER trip, or specialist appointment. Keep the most current version on your phone and printed copies in your wallet, purse, and at home. Outdated lists cause errors.
Can I get help from my local pharmacy?
Absolutely. Most pharmacies have pharmacists available for free consultations without an appointment. Ask for a Medication Therapy Management session. Bring the full list. Ask about drug interactions, simplifying the schedule, or switching to generics. Many now offer caregiver support hours. Walgreens and CVS have dedicated programs. Don’t wait for the doctor-go to the pharmacy first.
Is it okay to use someone else’s leftover pills?
No. Never. Even if the pill looks the same, the dosage, brand, or inactive ingredients may differ. Taking someone else’s meds can cause serious harm or death. If a person runs out, call the pharmacy or doctor. Don’t improvise. It’s not worth the risk.




