Medication Interaction Risk Checker
Check Your Medication Risks
Important Notes
This tool provides general information and is not a substitute for medical advice. Always consult with your doctor or pharmacist before making any changes to your medications.
Most dangerous interactions involve statins combined with drugs that inhibit CYP3A4 enzyme (like certain antibiotics and antifungals).
When you take two medications together, you might not think about how they could tear your muscles apart. But that’s exactly what can happen with rhabdomyolysis-a rare, dangerous condition where muscle cells break down and spill their contents into your blood. It’s not just about overdoing it at the gym. In fact, the biggest cause today isn’t injury or extreme exercise. It’s drug interactions.
What Happens When Muscles Start Breaking Down
Your muscles are made of cells packed with proteins, electrolytes, and enzymes. When something damages those cells-like a bad combo of pills-their insides leak out. The most dangerous of these is myoglobin, a protein that turns your urine dark brown or cola-colored. Your kidneys aren’t built to handle it. They get clogged, and that’s when things turn critical.Up to half of people with severe rhabdomyolysis develop acute kidney injury. Some need dialysis. About 5 to 15% die if their kidneys fail. The signs? Muscle pain, weakness, and dark urine. But here’s the catch: only about half of people notice all three. Many just feel tired, nauseous, or have vague back or shoulder pain. By the time they go to the ER, it’s often too late.
The Real Culprits: Statins and the Drugs That Make Them Deadly
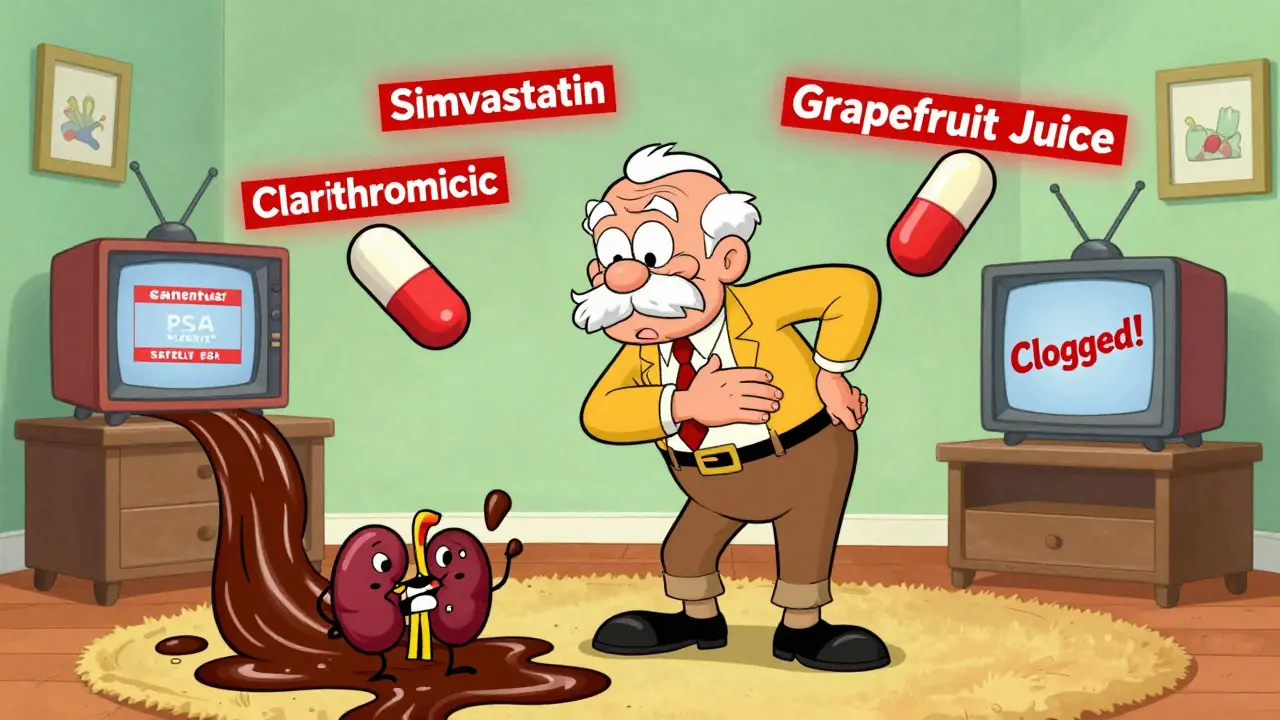
Statins-like Lipitor and Zocor-are the most common trigger. They lower cholesterol and save lives. But they’re also responsible for about 60% of all medication-induced rhabdomyolysis cases. The problem isn’t the statin alone. It’s what you take with it.Take simvastatin and gemfibrozil together. That combo increases your risk by 15 to 20 times compared to taking simvastatin by itself. Why? Both are processed by the same liver enzyme, CYP3A4. When one blocks it, the other builds up in your blood like a clogged pipe. The same thing happens with erythromycin, clarithromycin, itraconazole, or even grapefruit juice. These aren’t rare interactions. They’re textbook.
One patient in Birmingham, 72, was on simvastatin for years. Then his doctor added clarithromycin for a sinus infection. Within 48 hours, his urine turned dark. His CK level-the marker for muscle damage-spiked to 28,500 U/L. Normal is under 200. He spent three days in the hospital on IV fluids and nearly lost his kidneys.
Other Dangerous Drug Pairs You Might Not Know About
It’s not just statins. Other common meds can cause the same problem when mixed:- Colchicine + clarithromycin: Used for gout and infections, this combo increases rhabdomyolysis risk by 14 times. The European Medicines Agency issued a formal warning in 2021 after reviewing over 1,200 cases.
- Zidovudine (Retrovir) + other HIV drugs: In HIV patients, up to 12% develop significantly elevated CK levels when on this antiviral.
- Erlotinib + simvastatin: A cancer drug paired with a statin can cause CK levels over 20,000 U/L in under 72 hours. This combo is so dangerous that doctors in the U.S. now screen for it before prescribing.
- Leflunomide (for rheumatoid arthritis) + statins: Rare, but when it happens, CK levels can exceed 50,000 U/L. Plasma exchange is often needed because the drug stays in your body for weeks.
- Propofol (an IV anesthetic): In ICU patients, this can trigger a deadly syndrome that shuts down muscle energy production. Mortality hits 68% if rhabdomyolysis develops.
These aren’t edge cases. They’re documented in peer-reviewed journals, FDA reports, and hospital case files. And they’re avoidable-if you know to look.
Who’s Most at Risk?
Some people are far more likely to develop this. Age matters. If you’re over 65, your risk is more than three times higher. Women are 1.7 times more likely than men. If you have kidney problems-even mild ones-your risk jumps by 4.5 times.But the biggest factor? Polypharmacy. Taking five or more medications? You’re 17 times more likely to develop drug-induced rhabdomyolysis. That’s not a guess. It’s from a 2022 JAMA study tracking over 80,000 patients. Elderly patients on statins, blood pressure meds, painkillers, and antibiotics are sitting ducks.
There’s also a genetic angle. About 1 in 5 Europeans carry a gene variant called SLCO1B1*5. It makes them far more sensitive to simvastatin. Without testing, doctors have no way of knowing who’s at higher risk-unless they ask about unexplained muscle pain.
What Doctors Miss (And What You Should Watch For)
Most patients don’t connect muscle soreness to their meds. They think it’s just aging, or a new workout. A 2022 Reddit analysis of 147 rhabdomyolysis cases found that 92% of patients said their doctors never warned them the symptoms could be serious.Here’s what you should do:
- If you start a new medication-especially an antibiotic, antifungal, or heart drug-and you get unexplained muscle pain, weakness, or dark urine, stop the new drug and call your doctor today.
- Don’t wait for symptoms to get worse. CK levels can double in 24 hours.
- Keep a list of every pill you take, including supplements. Bring it to every appointment.
- Ask: “Could this new medicine interact with anything I’m already taking?” Don’t assume they checked.
Many doctors rely on electronic alerts. But those systems are flawed. They miss combinations if the drugs are prescribed by different specialists. You’re the only one who sees the full picture.
How It’s Treated-And Why Speed Matters
If rhabdomyolysis is caught early, treatment is straightforward: stop the bad combo and give lots of IV fluids. The goal? Flush out the myoglobin before it kills your kidneys. Doctors aim for urine output of 200-300 mL per hour. That’s about a cup every 20 minutes.In moderate to severe cases (CK over 5,000 U/L), hospitals add sodium bicarbonate to the IV to keep the urine alkaline. This prevents myoglobin from clumping in the kidneys. Some patients need dialysis. Others get plasma exchange if the drug has a long half-life, like leflunomide.
But the real win? Prevention. A 2021 Cleveland Clinic protocol shows that patients who get fluids within 6 hours of symptom onset are 70% less likely to need dialysis.

The Bigger Picture: Why This Is Getting Worse
We’re living longer, taking more pills, and seeing more specialists. The average 70-year-old in the UK now takes 6-8 medications. Every new prescription adds risk. The FDA’s Sentinel system saw a 22.4% spike in rhabdomyolysis reports after remdesivir was rolled out for COVID-19. That’s a new drug, new interactions, new cases.Regulators are catching up. The EMA now requires all statin labels to list specific drug contraindications. But hospitals still don’t routinely test for SLCO1B1*5. Pharmacists don’t always flag combinations. Patients aren’t educated.
Meanwhile, research is moving forward. The NIH is funding a real-time drug interaction alert system. Clinical trials are testing drugs that protect mitochondria from statin damage. But none of that helps you today.
Recovery and Long-Term Effects
If you survive, recovery isn’t quick. In cases without kidney damage, muscles usually heal in 12 weeks. But if you needed dialysis? That can stretch to 28 weeks or longer. About 44% of survivors still feel weak six months later.And the fear lingers. Many patients avoid statins even when they need them. That’s dangerous too-heart attacks are far more common than rhabdomyolysis. The key is balance. Don’t stop your meds. But do know the risks. Talk to your pharmacist. Ask for a medication review.
Can rhabdomyolysis happen from one medication, or only from interactions?
It can happen from a single drug, especially high-dose statins or drugs like colchicine or propofol. But most serious cases-especially fatal ones-are caused by interactions. About 89% of fatal rhabdomyolysis cases involve two or more drugs, according to the Journal of the American College of Cardiology.
What should I do if I notice dark urine after starting a new pill?
Stop the new medication immediately and go to urgent care or the ER. Don’t wait. Dark urine is a red flag for myoglobin in your blood. Get a creatine kinase (CK) blood test right away. If your CK is over 1,000 U/L, you likely have rhabdomyolysis. Early treatment prevents kidney failure.
Are all statins equally risky for rhabdomyolysis?
No. Simvastatin and lovastatin carry the highest risk, especially when combined with CYP3A4 inhibitors. Atorvastatin is safer, and pravastatin/rosuvastatin have the lowest risk because they’re not processed by that liver enzyme. If you’re on a high-risk statin and need an antibiotic, ask if you can switch to a safer statin first.
Can I take grapefruit juice with my statin?
No, not if you’re on simvastatin, lovastatin, or atorvastatin. Grapefruit juice blocks the same liver enzyme (CYP3A4) as many antibiotics and antifungals. Even one glass can raise statin levels by 300%. If you love grapefruit, ask your doctor if you can switch to pravastatin or rosuvastatin-they’re unaffected.
Is there a blood test to check if I’m genetically at risk?
Yes. The SLCO1B1 gene test can show if you’re more likely to develop muscle damage from simvastatin. It’s not routine yet, but it’s available through specialized labs. If you’re over 65, have kidney issues, or have had muscle pain on statins before, ask your doctor about testing. It could prevent a hospital stay.
What to Do Next
If you’re on more than three medications, especially if you’re over 65 or have kidney problems, schedule a medication review with your pharmacist. Bring your pill bottles or a list. Ask: “Could any of these cause muscle damage together?”Don’t wait for symptoms. Don’t assume your doctor checked. Rhabdomyolysis is rare-but it’s preventable. And when it strikes, time is everything.