Antidepressant — What You Need to Know Right Now
Antidepressants can help lift mood, reduce anxiety, and make daily life easier — but they’re not one-size-fits-all. If you’re reading this because you or someone you care about is starting, switching, or worried about interactions, this page gives straightforward, practical info you can use in a conversation with your clinician.
How antidepressants work and common types
Most antidepressants change brain chemicals that affect mood. The main classes you’ll hear about are SSRIs (like sertraline), SNRIs (like venlafaxine), TCAs (like imipramine), and MAOIs (used less often). Each group works differently, so side effects and time to feel better vary. SSRIs often take 4–6 weeks for full effect; SNRIs can help both mood and certain pain types; TCAs work but have more side effects; MAOIs need strict dietary rules.
When choosing one, doctors look at your symptoms, other medical conditions, current meds, and past responses. If pain or nerve symptoms are present, some antidepressants double as pain treatments. If sleep is a problem, some options are more sedating. Talk about what matters most to you — sleep, energy, or side effects — so your prescriber can pick a better match.
Interactions, side effects, and practical tips
Drug and herb interactions are a real issue. For example, St. John’s wort can interfere with many prescriptions and may reduce blood levels of drugs or add to serotonin-related risks. Herbs like valerian and kava can increase drowsiness when mixed with some antidepressants. If you take imipramine or other TCAs, mention any supplements to your doctor — we cover this in our post about herbal interactions with imipramine.
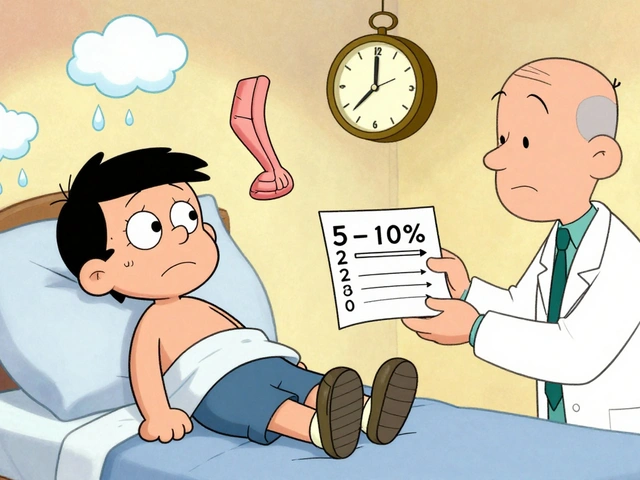
Watch for common side effects: nausea, sleep changes, sexual issues, dry mouth, and dizziness. Some side effects fade after 1–2 weeks; sexual side effects and weight changes may take longer. More urgent signs — severe agitation, high fever, fast heartbeat, or muscle stiffness — need immediate care because they can signal rare but serious reactions like serotonin syndrome.
Practical tips: always tell your provider about every medicine and supplement you take; avoid stopping suddenly — many drugs need a gradual taper; set a follow-up at 2–4 weeks after a change so side effects and response can be checked. If cost or access is a problem, look at trusted alternatives and RX savings programs before switching; we have guides on alternatives and online pharmacy options on this site.
Non-drug options matter too. Therapy, regular exercise, sleep routines, and mindfulness or yoga can boost results and help prevent relapse. If medication feels like the only tool offered, ask about combining it with talk therapy or lifestyle changes — we summarize how yoga and meditation can help with major depressive disorder in a separate article.
If you want more detail, check our posts on imipramine and herbs, yoga for depression, and comparisons of meds for pain and mood. Use those pieces to bring specific questions to your clinician — the right conversation makes treatment safer and more effective.