COPD Flare-Up: What Causes It, How to Spot It, and What to Do
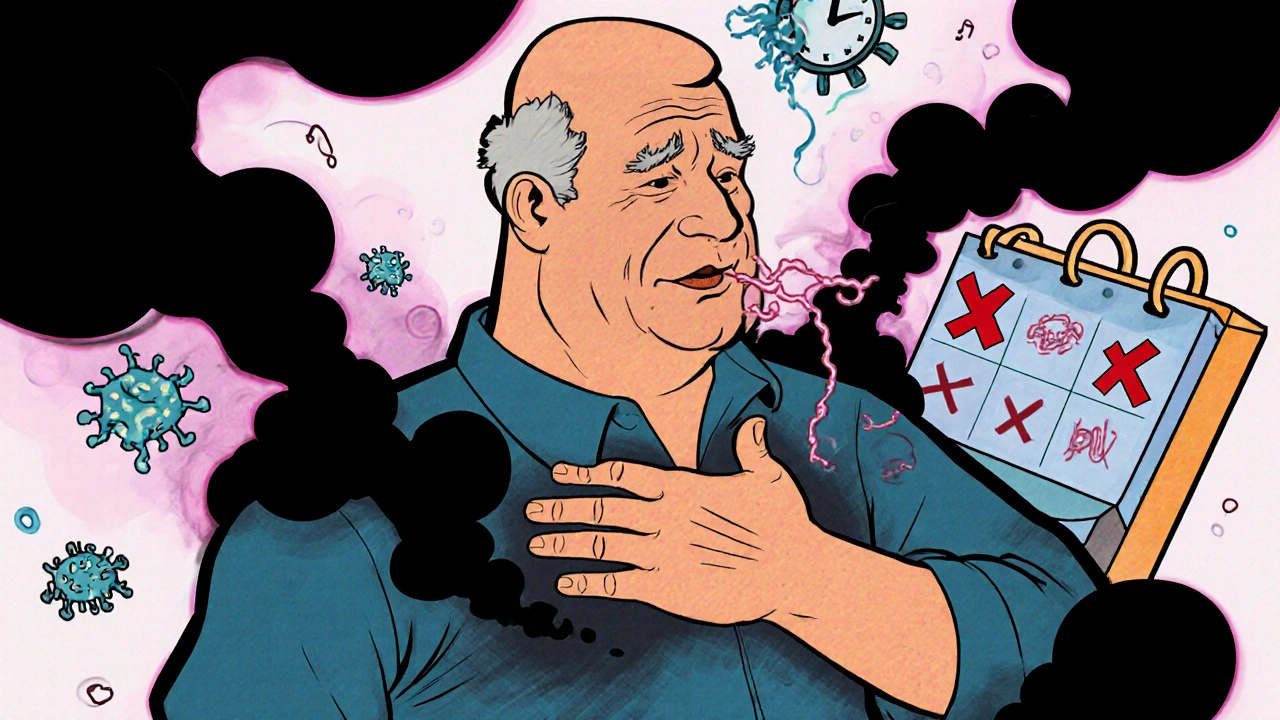
When your lungs suddenly feel tighter than usual, and breathing becomes a chore even sitting still, you might be facing a COPD flare-up, a sudden worsening of chronic obstructive pulmonary disease symptoms that often requires urgent care. Also known as an exacerbation, this isn’t just a bad day—it’s your body signaling that something has pushed your lungs past their limit. These episodes don’t come out of nowhere. They’re usually triggered by infections like colds or flu, air pollution, or even skipping your daily meds.
People with chronic obstructive pulmonary disease, a long-term lung condition that includes emphysema and chronic bronchitis, making it hard to breathe know the quiet dread that comes with a change in cough, mucus color, or shortness of breath. A flare-up might start with more phlegm than usual—especially if it turns yellow or green—or a sudden need for your rescue inhaler. Some notice swelling in their ankles, confusion, or feeling too tired to get out of bed. These aren’t normal ups and downs. They’re red flags.
What makes a COPD flare-up dangerous isn’t just the breathlessness—it’s how fast it can spiral. Many people wait too long to act, thinking it’ll pass. But studies show that early treatment cuts hospital stays by nearly half. That’s why knowing your personal warning signs matters more than generic advice. If your usual meds aren’t helping, or you’re using your inhaler more than twice a day, it’s time to call your doctor. Sometimes, a short course of steroids or antibiotics can stop it before it becomes a full-blown emergency.
Managing COPD treatment, the ongoing plan that includes medications, oxygen, pulmonary rehab, and lifestyle changes to slow disease progression isn’t just about daily pills. It’s about recognizing the early signs of trouble and having a clear plan. That’s why many people keep a written action plan—what to do when symptoms start, who to call, and when to go to the ER. It’s the same logic behind organizing a medication list for caregivers: preparation saves lives.
And while COPD is often linked to smoking, it’s not the only cause. Long-term exposure to dust, chemicals, or even secondhand smoke can trigger it. That’s why even non-smokers can have flare-ups—and why avoiding triggers like cold air, strong perfumes, or wildfire smoke is part of the daily routine.
Below, you’ll find real-world guides on how to manage medications, recognize dangerous side effects, and work with your care team to avoid hospital visits. Whether it’s understanding how drug interactions affect your lungs or learning how to track symptoms before they explode, these posts give you the tools to stay in control—before the next flare-up hits.