COPD Symptoms: What to Watch For and How to Manage Them
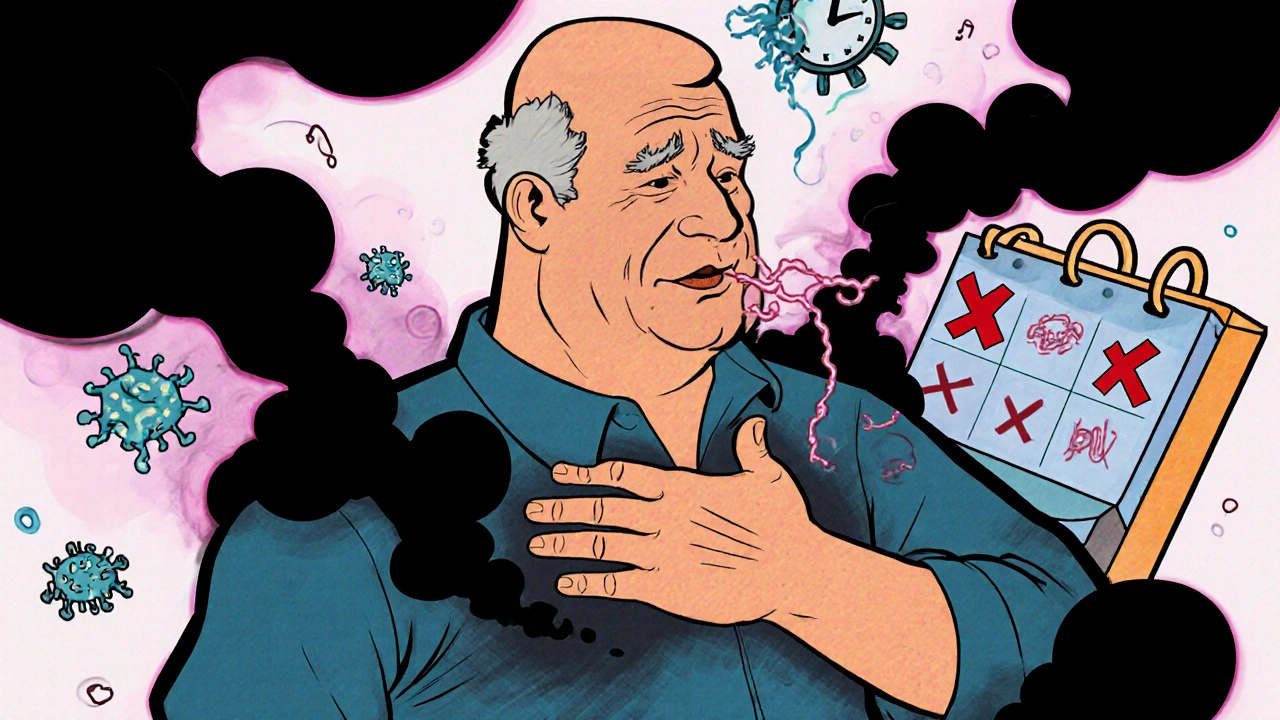
When you have COPD, Chronic Obstructive Pulmonary Disease is a group of lung conditions that make it hard to breathe, often due to long-term damage from smoke or pollution. Also known as chronic bronchitis and emphysema, it doesn’t go away—but knowing the signs helps you take control before it gets worse. Most people ignore the early warning signs, thinking it’s just aging or being out of shape. But if you’re constantly winded after walking up stairs, coughing up mucus every morning, or feeling tightness in your chest after light activity, those aren’t normal. They’re your lungs telling you something’s wrong.
Chronic bronchitis, a type of COPD where the airways are inflamed and produce too much mucus means you’ll likely have that nagging cough for months, especially in cold or damp weather. Emphysema, the other main form of COPD, destroys the air sacs in your lungs so they can’t push air out properly, leaving you breathless even at rest. These two often overlap, and together they make simple tasks like tying your shoes or carrying groceries exhausting. You might also notice wheezing, frequent respiratory infections, or blue-tinged lips and fingernails when your body isn’t getting enough oxygen.
What’s rarely talked about is how COPD symptoms creep in slowly. Many people wait years before seeing a doctor because they think breathing harder is just part of getting older. But the damage is already happening. And the longer you wait, the harder it becomes to slow it down. The good news? Catching it early means you can use medications, breathing exercises, and lifestyle changes to keep your lungs working better for longer. You can still walk, travel, and enjoy time with family—you just need to know what’s going on inside your body.
Below, you’ll find real-world advice from people managing COPD every day. From organizing medications to spotting when a flare-up is coming, these posts give you practical steps—not just theory. You’ll learn how to track symptoms, avoid triggers, and work with your care team to stay out of the hospital. This isn’t about fear. It’s about knowing what’s happening so you can act before it’s too late.