Emergency COPD Treatment: What Works Fast and What to Avoid
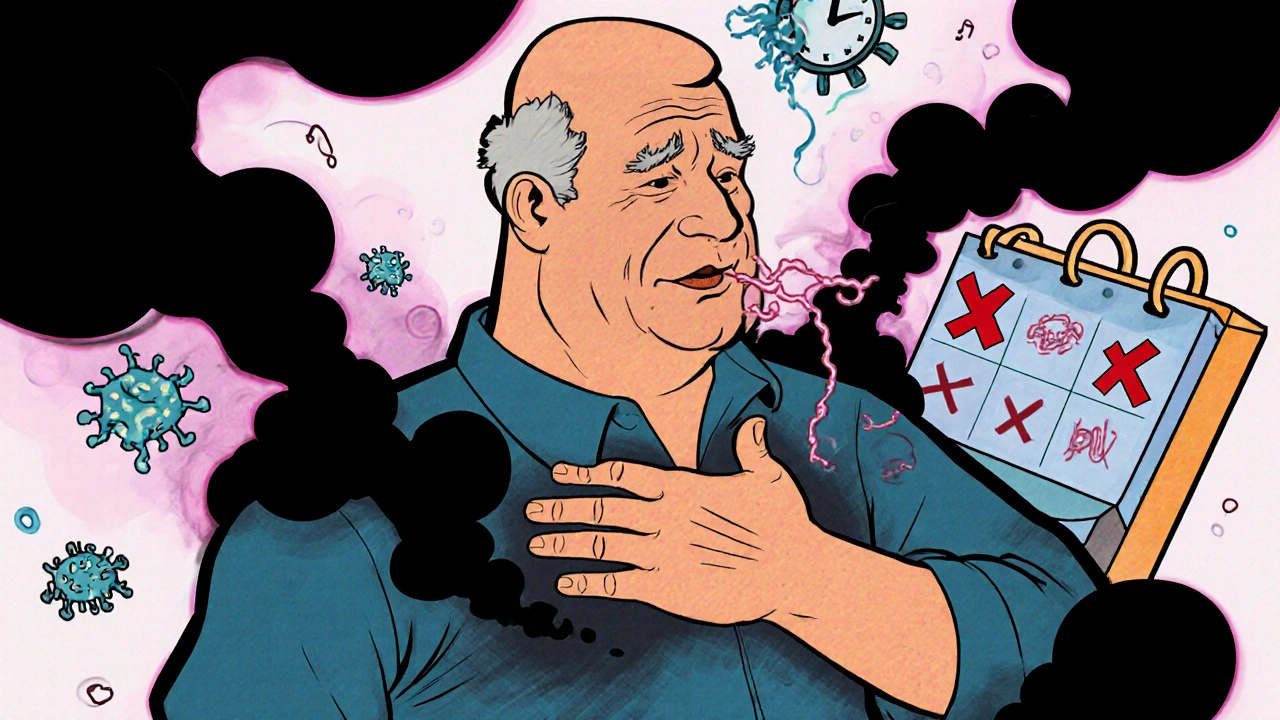
When someone with COPD, Chronic Obstructive Pulmonary Disease, a progressive lung condition that makes breathing difficult. Also known as chronic bronchitis or emphysema, it often flares up without warning. has an emergency COPD treatment situation, seconds matter. A sudden spike in breathlessness, wheezing, or confusion isn’t just uncomfortable—it’s dangerous. This isn’t the time to wait and see. Quick, correct action can stop a trip to the ER or even save a life.
Most emergency COPD treatments start with bronchodilators, medications that relax the airway muscles to open up breathing passages. Inhaled forms like albuterol or ipratropium are the first line—they work in minutes. If you’ve been prescribed a rescue inhaler, use it right away. If symptoms don’t improve after two puffs, call for help. Many people skip this step, hoping it’ll pass, but delays can lead to respiratory failure. Oxygen therapy is another critical tool in emergencies. Not everyone with COPD needs constant oxygen, but during a flare-up, low blood oxygen levels can cause organ damage. Emergency responders and hospitals use controlled oxygen to bring levels back up safely—too much can backfire, which is why it’s never a DIY fix.
Other common treatments include corticosteroids, anti-inflammatory drugs that reduce airway swelling during acute flare-ups. These are often given orally or intravenously in hospitals to calm the body’s overreaction. Antibiotics may be added if infection—like pneumonia or a bad cold—is the trigger. But not every flare-up needs them. Overusing antibiotics leads to resistance and doesn’t help if the cause is pollution, stress, or cold air. The key is identifying the cause fast. That’s why keeping a symptom log helps your doctor decide what to do next time.
What you should never do in an emergency: reach for an old prescription without checking with a professional, try home remedies like steam or essential oils, or wait until you’re too weak to call 911. COPD flare-ups don’t always look like the movies—sometimes it’s just a quiet, worsening exhaustion. If you’re using your rescue inhaler more than usual, or you can’t speak in full sentences, that’s your signal. This isn’t about being dramatic—it’s about recognizing the body’s warning signs before it’s too late.
The posts below cover what happens after the emergency, how to prevent the next one, and what medications and tools actually help. You’ll find real advice on managing daily symptoms, avoiding triggers, and knowing when to act before things spiral. No fluff. Just what works.