Meniere's Disease: Recognize Symptoms and Manage Attacks
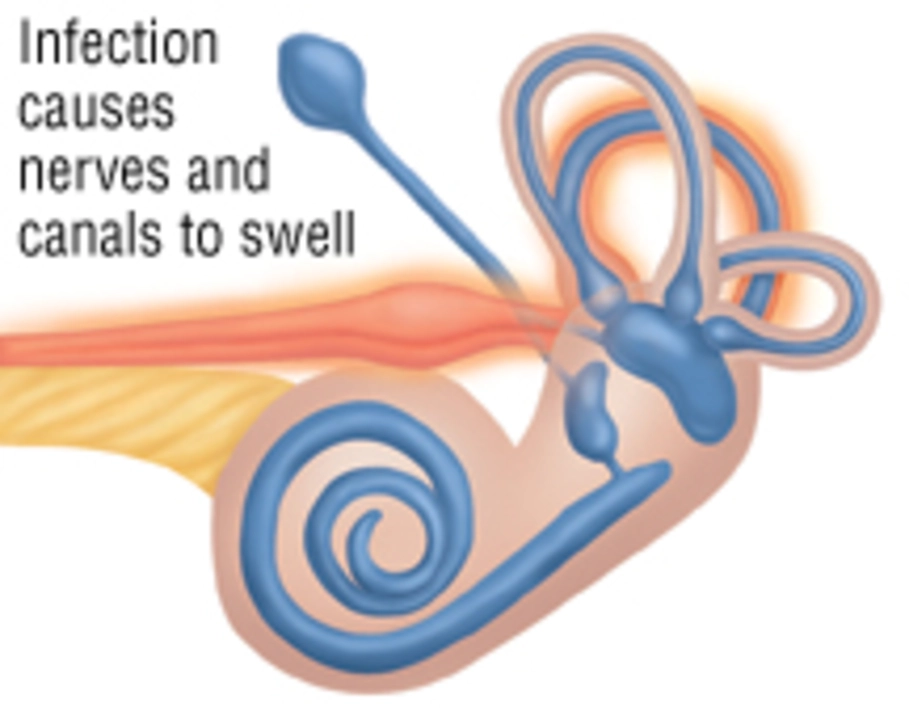
Ever had a sudden room-spinning attack, ringing in the ear, and pressure like your ear is full? Those are classic signs of Meniere's disease. It’s an inner-ear condition that causes recurring vertigo episodes, fluctuating hearing loss, tinnitus, and a feeling of fullness in one ear. Not everyone has the same pattern, so tracking what happens and when really helps your doctor.
Symptoms & Diagnosis
Vertigo in Meniere's usually comes in sudden attacks that last 20 minutes to several hours. Between attacks, hearing can improve or stay worse—over time many people notice permanent hearing loss on the affected side. Tinnitus (constant or intermittent ringing) and a sensation of fullness in the ear often show up early.
Doctors confirm Meniere's with an audiogram (hearing test) showing fluctuating low- to mid-frequency hearing loss. They may order vestibular tests (VEMP, ENG) to check balance function and an MRI to rule out other causes like vestibular schwannoma. A symptom diary—dates, length of attacks, what you ate or did—gives your clinician useful clues.
Treatment Options and Everyday Tips
There’s no single cure, but treatments aim to reduce attack frequency and protect hearing. For sudden vertigo, short-term meds like meclizine or diazepam can ease nausea and dizziness. For longer-term control, a low-sodium diet and diuretics (under a doctor’s guidance) often help by reducing inner-ear fluid pressure.
When meds and diet aren’t enough, ENT specialists may offer targeted procedures. Intratympanic steroid injections can calm inflammation and reduce attacks for many people. Intratympanic gentamicin is more aggressive; it reduces vertigo by weakening ear balance function but risks more hearing loss. Surgical options like endolymphatic sac decompression are considered when conservative care fails and hearing is still useful.
Vestibular rehabilitation (balance therapy) teaches your brain to cope with inner-ear changes. If hearing loss becomes permanent, hearing aids or bone-conduction devices can make a big difference. Cochlear implants are an option in severe bilateral loss.
Practical tips you can use today: keep a low-salt diet, limit caffeine and alcohol, stay hydrated, get regular sleep, and manage stress—those things lower attack chances. During an attack, sit or lie down, focus on a fixed point, avoid bright lights or sudden head turns, and don’t drive. Carry anti-nausea meds if prescribed.
If you notice sudden severe imbalance, double vision, weakness, or slurred speech, get emergency care—those signs need immediate evaluation. Otherwise, plan visits with an ENT and audiologist, bring your diary, and ask about vestibular therapy or steroid injections if attacks continue.
Living with Meniere's means learning your triggers and building a simple routine to reduce attacks and protect hearing. Small changes—salt control, good sleep, tracking symptoms—often add up to fewer bad days and better long-term outcomes.