Parkinson's Disease: Practical Guide to Symptoms, Treatment, and Daily Life
Do you worry about a tremor, slow movement, or that constant stiffness? Parkinson's disease (PD) often starts quietly and changes daily life bit by bit. This page gives clear, useful steps you can take—what to watch for, how doctors diagnose it, treatment basics, and simple daily tips to feel more in control.
Spotting symptoms early
Motor signs are the ones people notice first: a resting tremor (often in one hand), slowness of movement (bradykinesia), stiffness (rigidity), and balance problems. Non-motor signs are common too—loss of smell, constipation, sleep problems, mood changes, and low blood pressure when standing. If you notice a steady pattern of these changes, bring a list of symptoms to your doctor with examples of when they happen.
Don’t wait for all symptoms to appear. Even mild tremor or new stiffness that interferes with dressing, typing, or walking is worth checking. Early diagnosis helps you get treatments that improve quality of life.
Treatment options that work in real life
There’s no cure yet, but many treatments help you move better and stay active. Levodopa (usually combined with carbidopa) remains the most effective medication for reducing slowness and stiffness. Other drugs—dopamine agonists, MAO-B inhibitors, and COMT inhibitors—can help in specific cases or delay levodopa use.
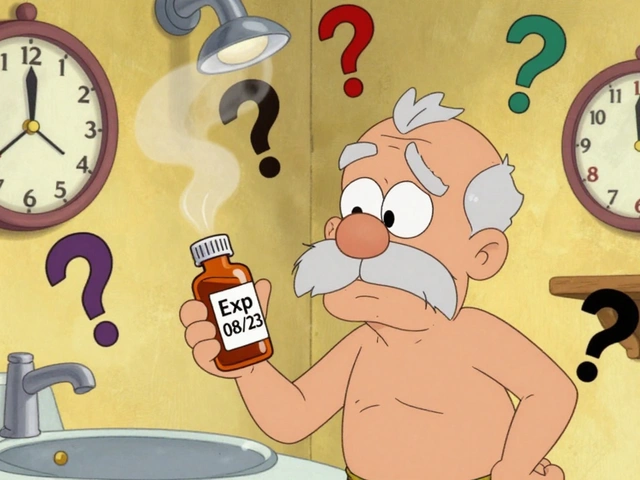
Medication timing matters. Keep a daily log of when symptoms worsen and when you take meds. Protein-heavy meals can reduce levodopa absorption; try spacing large protein meals away from dosing times. Use a pill box or alarm to avoid missed doses, and always carry a current medication list.
If meds stop working well or cause involuntary movements (dyskinesia), talk to your neurologist. Options include changing doses, adding meds, or advanced treatments like deep brain stimulation (DBS) for the right candidates.
Exercise is one of the best daily tools. Aim for regular aerobic activity—walking, cycling, or swimming—and add balance and strength training. Big, fast movements help retrain the brain; local programs like boxing for Parkinson’s show real benefits. Speech therapy (LSVT LOUD) helps voice and swallowing problems. Occupational therapists teach safer ways to dress, cook, and move at home.
Small home changes cut risk: add grab bars, remove loose rugs, improve lighting, and use non-slip mats. For daytime fatigue, break tasks into short chunks and sit to put on shoes or shave. Caregivers: encourage routines, keep emergency contacts handy, and join a local support group—sharing tips matters.
When to see a specialist? If symptoms affect daily tasks, worsen over weeks, or if medications cause troubling side effects, ask for a movement disorder neurologist. They focus on Parkinson’s and can tailor a plan that fits your life.
Parkinson’s is manageable with the right mix of medicine, therapy, and daily routines. Track symptoms, stay active, and lean on your health team—small changes often bring big improvements.