Psychiatric Drug Interactions: Risks, Common Combinations, and What to Watch For
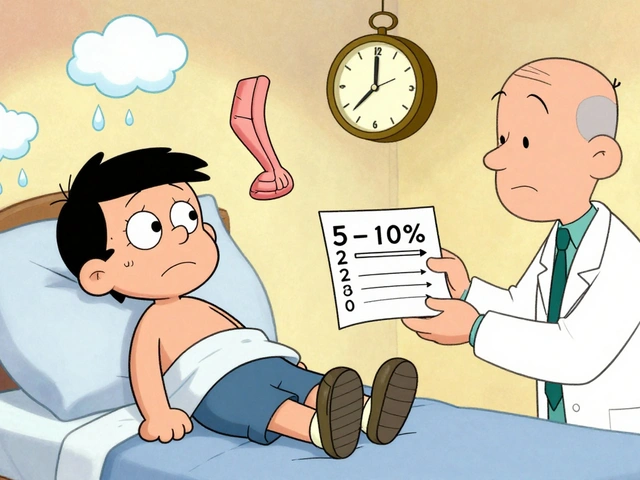
When you're taking psychiatric drug interactions, harmful overlaps between medications used to treat mental health conditions. Also known as psychotropic drug clashes, they happen when two or more drugs affect the same body systems in ways that increase side effects or reduce effectiveness. This isn’t rare—nearly 1 in 3 adults on antidepressants or antipsychotics are also taking other meds that could clash. The risk goes up sharply if you’re managing more than one mental health condition, or if you’re older and dealing with other chronic issues like high blood pressure or diabetes.
Antipsychotics, medications like olanzapine, clozapine, and lurasidone used for schizophrenia and bipolar disorder are especially tricky. They slow down how your liver breaks down other drugs, which can cause dangerous buildup. For example, mixing certain antipsychotics with SSRIs like sertraline (Zoloft) or fluoxetine (Prozac) can spike serotonin levels too high—leading to serotonin syndrome, a life-threatening reaction with symptoms like confusion, rapid heartbeat, and muscle rigidity. Even over-the-counter sleep aids or cough syrups can add to the danger. Antidepressants, drugs like SSRIs, SNRIs, and bupropion used to treat depression and anxiety aren’t safe just because they’re common. Combining them with MAO inhibitors (even in some herbal supplements) can cause sudden, severe spikes in blood pressure.
Polypharmacy—taking five or more medications—is a major red flag. It’s common in older adults with depression, dementia, or chronic pain, but each extra pill multiplies the chance of a bad interaction. Some combinations are silent killers: antipsychotics plus diuretics can cause dangerous electrolyte shifts; benzodiazepines with opioids can shut down breathing. You won’t always feel it coming. That’s why keeping a real, updated list of every pill, patch, or supplement you take is non-negotiable. Doctors miss interactions all the time—especially if you don’t mention that you’re taking St. John’s wort or melatonin. The good news? Most of these risks are avoidable. A simple check with your pharmacist or a quick review of your full med list can prevent hospital visits.
What you’ll find below are real, practical guides from people who’ve been there—how to spot the warning signs of a dangerous mix, which meds are most likely to cause trouble, how to talk to your doctor without sounding paranoid, and what to do if you start feeling off after a new prescription. These aren’t theory pieces. They’re checklists, comparisons, and step-by-step advice from patients and clinicians who’ve seen the fallout—and know how to stop it before it starts.