Senior Medications: Safe Choices, Common Risks, and What to Watch For
When you’re over 65, your body handles senior medications, drugs prescribed to older adults to manage chronic conditions like high blood pressure, diabetes, or arthritis. Also known as geriatric pharmacology, this field focuses on how aging changes the way your body absorbs, processes, and gets rid of drugs. It’s not just about taking more pills—it’s about understanding why some medicines that work fine for younger people can cause falls, confusion, or kidney trouble in seniors.
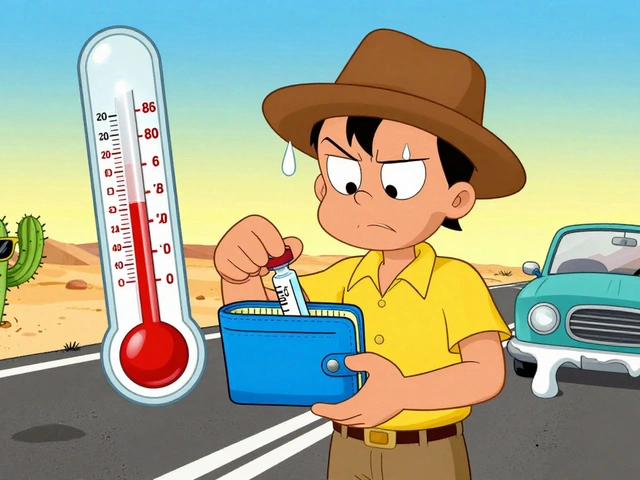
Many older adults take polypharmacy in seniors, the use of five or more medications at once. Also known as multiple drug regimens, it’s common because conditions like heart disease, arthritis, and diabetes often show up together. But each new drug adds risk. For example, combining a diuretic with an anticholinergic—both common in seniors—can raise your chance of heat stroke or dizziness. Or mixing an SSRI with an NSAID might lead to internal bleeding. The elderly drug interactions, harmful overlaps between medications that affect older adults differently than younger people. Also known as age-related drug conflicts, they’re often missed because symptoms like fatigue or memory lapses get blamed on aging itself.
Some drugs are simply riskier for seniors. Antipsychotics like olanzapine can trigger weight gain and diabetes. Benzodiazepines for sleep might lead to falls and fractures. Even common painkillers like ibuprofen can damage kidneys or raise blood pressure. And let’s not forget how easy it is to overlook age-related medication side effects, changes in how the body reacts to drugs as you get older, including slower metabolism and reduced kidney function. Also known as geriatric adverse reactions, they don’t always look like typical side effects—sometimes it’s just feeling off, forgetting to eat, or losing balance. These aren’t rare. Studies show nearly half of seniors on multiple meds experience at least one avoidable side effect.
What’s missing from most doctor visits? A full review. Too often, each specialist adds a drug without seeing the full list. That’s why it’s so important to bring all your pills—supplements included—to every appointment. Ask: Is this still needed? Could something else work with fewer risks? Are there generics that are just as safe? You’re not being difficult—you’re protecting your health.
The posts below cover real cases and practical advice: how SGLT2 inhibitors can cause yeast infections in older diabetics, why certain psychiatric drugs clash dangerously, how heat affects those on diuretics, and what to do when a medication stops working—or starts causing new problems. You’ll find clear breakdowns of what works, what doesn’t, and what to ask your pharmacist before the next refill. This isn’t theory. It’s what happens when prescriptions pile up—and how to keep things under control.