Tolerance Mechanisms Explained
When dealing with tolerance mechanisms, the biological processes that reduce a drug’s effect over time. Also known as drug tolerance, these mechanisms can involve changes at the cellular level, shifts in metabolism, or even altered brain signaling. Understanding them helps you see why a medication that once worked well might need a higher dose or a switch to a different class.
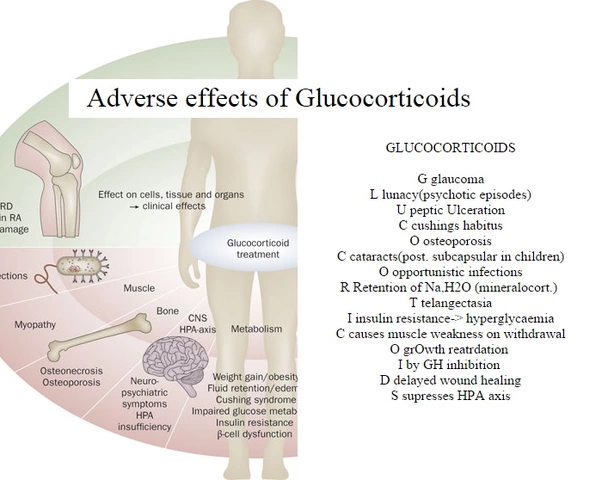
One of the core players is receptor desensitization, the reduced responsiveness of receptors after repeated exposure. When a drug repeatedly binds to its target, the receptor can become less active or be pulled into the cell, leading to a weaker response. This pharmacodynamic tolerance often forces clinicians to adjust dosages, as seen in many of the articles below about antidepressants, antihistamines, and pain relievers. Another major factor is enzyme induction, the accelerated breakdown of drugs by liver enzymes. Enzyme induction speeds up metabolism, so the same dose clears faster, reducing its effect. Both receptor desensitization and enzyme induction illustrate the semantic triple: tolerance mechanisms encompass receptor desensitization; tolerance mechanisms require enzyme induction; and enzyme induction influences pharmacodynamic tolerance.
Why Tolerance Matters for Everyday Medications
Whether you’re taking a diuretic in summer heat, a steroid for skin conditions, or an antidepressant like Wellbutrin, tolerance can change the game. For instance, the heat‑safety article on diuretics warns that increased dehydration can amplify tolerance to the drug’s fluid‑removing effects, making dosing tricky. Similarly, the betamethasone skin piece highlights how long‑term steroid use can trigger receptor down‑regulation, a classic sign of tolerance that leads to skin thinning. Even non‑prescription supplements such as Brahmi or Nootropil face similar hurdles—your brain may adapt, dulling the initial boost in cognition.
Knowing the underlying mechanisms lets you anticipate adjustments before problems arise. If you notice diminishing benefits, ask your doctor about rotating medications, adding a drug-free interval, or using a different class that bypasses the same receptors. Some clinicians employ “tolerance‑breaks” to reset receptor sensitivity, a strategy seen in the management of chronic fatigue linked to hormonal imbalances. Others might combine therapies—like adding yoga for colitis relief—to reduce reliance on high‑dose drugs that provoke tolerance.
The collection of posts on this page reflects these ideas across a wide range of conditions: from hormone‑related alopecia to shift‑work disorder in healthcare workers, from infectious disease prevention to specialty drug comparisons. Each article touches on how tolerance mechanisms shape treatment outcomes, side‑effects, or the need for alternative strategies. Dive into the articles below to see real‑world examples of tolerance in action and learn practical steps you can take today.