Uterine Lining Overgrowth: Understanding, Risks, and Treatment Options
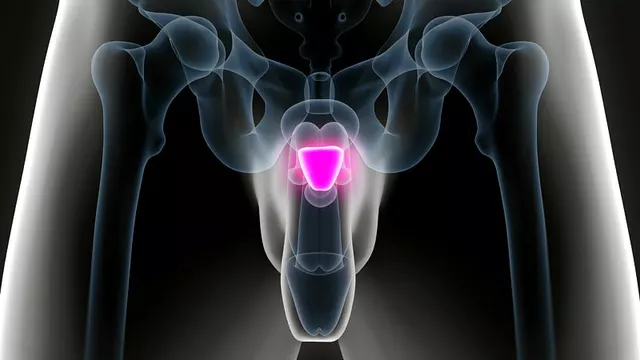
When dealing with uterine lining overgrowth, the thickening of the endometrial tissue beyond its normal cycle. Also known as endometrial hyperplasia, it often shows up as irregular spotting or heavy periods. In simple terms, the lining grows faster than it sheds, which can throw off the whole menstrual rhythm. This condition encompasses a range of sub‑issues, from mild cellular changes to precancerous states, and it usually signals that something in the hormonal balance is off.
What Drives the Overgrowth?
One of the biggest drivers is hormonal imbalance, especially excess estrogen without enough progesterone to counter it. When estrogen keeps the lining in a growth mode and progesterone fails to signal a break, the tissue can pile up. This imbalance can stem from factors like polycystic ovary syndrome, obesity, or even certain medications that raise estrogen levels. Another key player is progesterone therapy, which is often used to rebalance the cycle. Proper progesterone can thin the overgrown lining and lower the risk of turning into cancer. Besides hormones, age, genetics, and lifestyle habits such as diet and stress levels also shape how the lining behaves. Understanding these connections helps you spot early signs, like abnormal uterine bleeding, before they become a bigger problem.
Diagnosing uterine lining overgrowth typically means an ultrasound, a biopsy, or a simple office hysteroscopy. These tools let doctors see how thick the lining really is and whether the cells look normal. If the test shows simple hyperplasia, lifestyle tweaks—weight management, smoking cessation, and adjusting hormone‑affecting meds—can do a lot. For more serious cases, doctors might prescribe progestin pills, a hormonal IUD, or even targeted anti‑estrogen drugs. Regular monitoring is crucial because the condition can slip back if the hormonal environment changes. The articles below dive into related topics like medication tolerance, heat safety for certain drugs, and how hormonal shifts affect other health areas, giving you a broader picture of how everything ties together. Ready to explore practical steps, treatment options, and real‑world advice? Keep reading for the detailed guides that follow.