Birth Control & Vaginal Irritation Risk Calculator
Enter your details and click "Calculate Risk Level" to see personalized information about potential vaginal irritation risks associated with your birth control method.
When Vaginal irritation refers to redness, itching, burning, or unusual discharge in the vaginal area shows up after you start a new contraceptive, it’s easy to think the two are linked. The truth is a mix of hormone shifts, material contact, and changes in the natural vaginal ecosystem. If you’re battling vaginal irritation while using contraception, here’s what to know.
Key Takeaways
- Hormonal methods can alter the vaginal pH and increase susceptibility to yeast infections.
- Physical devices like IUDs or diaphragms may cause friction or allergic reactions.
- Good hygiene, compatible lubricants, and regular check‑ups reduce most irritation risks.
- Persistent symptoms-especially pain, foul odor, or heavy discharge-require a medical review.
- Different contraceptive types have distinct irritation profiles; choosing the right one matters.
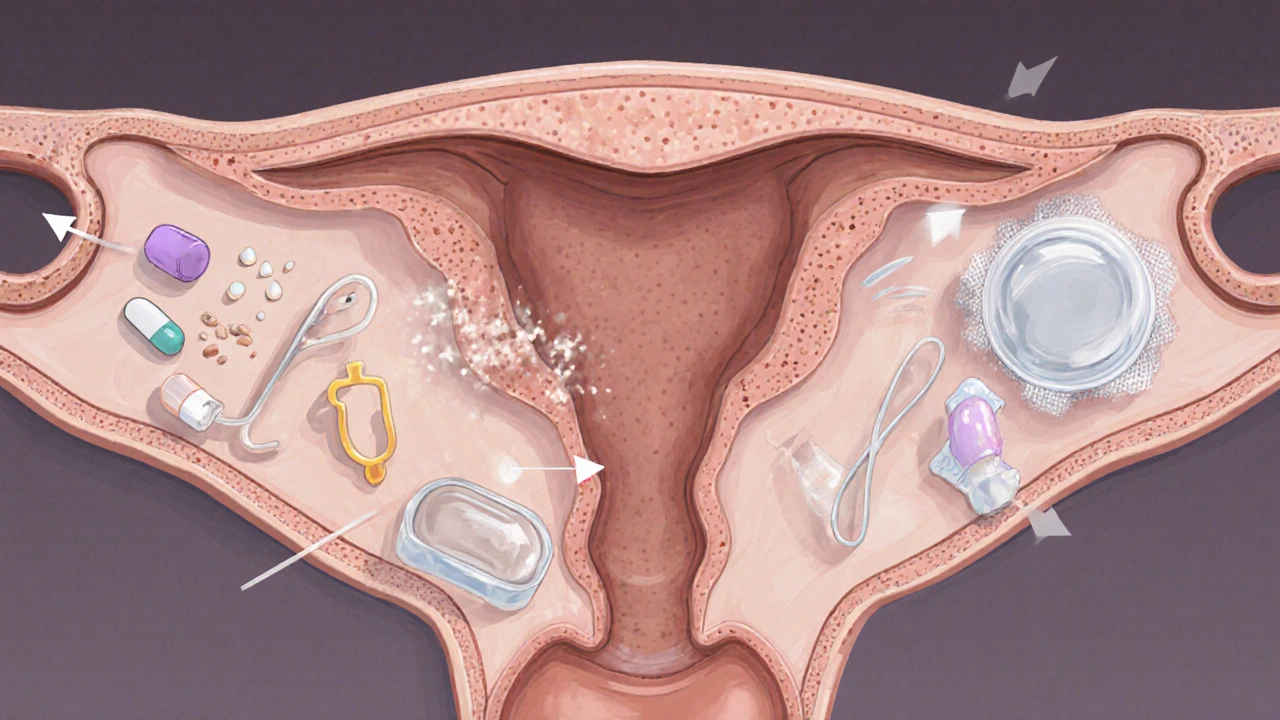
How Birth Control Can Trigger Irritation
Hormonal contraceptive includes pills, patches, rings, injections, and hormonal intrauterine devices that release estrogen and/or progestin changes the balance of estrogen and progesterone in your bloodstream. Those hormones also influence the growth of Lactobacillus beneficial bacteria that keep the vaginal environment slightly acidic. When estrogen drops, the acidity may rise, creating an environment where yeast thrives, leading to a yeast infection.
Physical methods such as the Copper IUD a small T‑shaped device placed in the uterus that releases copper ions to prevent pregnancy or contraceptive diaphragms sit close to the vaginal walls. If the device is not positioned correctly, it can rub against delicate tissue, causing micro‑abrasions and local inflammation.
Even non‑hormonal barriers like latex Condom a thin sheath worn over the penis to block sperm can trigger a latex allergy. Symptoms range from mild itching to intense swelling, and the allergic reaction often masquerades as generic irritation.
Common Causes of Vaginal Irritation with Contraceptives
- Yeast infection: Often linked to hormonal shifts caused by pills or the hormonal IUD. Look for thick, white “cottage‑cheese” discharge and itching.
- Bacterial vaginosis (BV): An overgrowth of anaerobic bacteria that changes vaginal odor. Certain hormonal combinations can lower protective lactobacilli, paving the way for BV.
- Allergic reaction: Latex, silicone, or even the copper in an IUD can provoke a localized allergy. Redness and a burning sensation are typical.
- Physical friction: Poorly fitted diaphragms, pessaries, or an incorrectly placed IUD can cause repetitive rubbing, especially during intercourse.
- Drying agents: Some spermicidal gels contain nonoxynol‑9, which can strip natural lubrication and leave the epithelium raw.
Which Contraceptive Methods Carry Higher Irritation Risk?
| Method | Typical irritation triggers | Average reported irritation rate |
|---|---|---|
| Combined oral pill | Hormone‑induced pH shift, yeast overgrowth | 12‑15% |
| Progestin‑only pill | Dryness, occasional BV | 8‑10% |
| Hormonal IUD (e.g., Mirena) | Local hormone release, occasional copper allergy | 5‑7% |
| Copper IUD | Physical irritation, copper allergy | 6‑9% |
| Condom (latex) | Latex allergy, friction | 2‑4% |
| Condom (polyurethane) | Reduced allergy risk, still possible friction | 1‑2% |
| Diaphragm | Improper fit, spermicide irritation | 7‑9% |
Practical Prevention Tips
- Choose the right material: If you have a known latex allergy, switch to polyurethane or polyisoprene condoms.
- Give hormonal methods a "settling period": Most mild irritation eases after two to three menstrual cycles. Keep track of symptoms.
- Maintain a balanced vaginal microbiome:
- Eat probiotic‑rich foods (yogurt, kefir, sauerkraut).
- Avoid douching; it disrupts natural flora.
- Consider a daily oral probiotic supplement if you’ve had recurrent BV.
- Use water‑based, fragrance‑free lubricants to reduce friction, especially with diaphragms or during intercourse.
- Schedule a follow‑up with your clinician after the first month of a new method to confirm proper placement (for IUDs) and to discuss any irritation.

When to Seek Professional Help
If any of these signs appear, make an appointment:
- Severe burning or pain that doesn’t improve after a few days.
- Yellow‑green or fishy‑smelling discharge (possible BV).
- Recurring yeast infections (more than three episodes per year).
- Visible rash, swelling, or blistering that spreads beyond the immediate contact area.
- Fever, pelvic pain, or abnormal bleeding after IUD insertion.
Your clinician may take a swab for lab analysis, check IUD positioning with ultrasound, or suggest a switch to a different contraceptive type.
Treatment Options Tailored to the Cause
Once the underlying trigger is identified, treatment is straightforward:
- Yeast infection: Over‑the‑counter azole creams (clotrimazole 1%) or a single‑dose oral fluconazole. Repeat the course if symptoms persist after 48‑72 hours.
- Bacterial vaginosis: Metronidazole gel 0.75% for five days or a single oral dose of tinidazole.
- Allergy: Discontinue the offending product, switch to a hypo‑allergenic alternative, and apply a mild corticosteroid cream for inflammation.
- Physical irritation: Ensure correct device placement, use a water‑based lubricant, and give the tissue 24‑48 hours of rest before resuming intercourse.
- Hormonal adjustment: If pills cause frequent irritation, ask your provider about a lower‑dose formulation or a non‑hormonal method.
Frequently Asked Questions
Can I use a hormonal IUD if I’ve had recurrent yeast infections?
Yes, but monitor symptoms closely. Some users experience fewer yeast episodes after the first few months as the local hormone dose stabilizes. If infections persist, discuss a switch to a copper IUD or a non‑hormonal option.
Is it safe to use spermicidal lubricants with condoms?
Most spermicides contain nonoxynol‑9, which can irritate the vaginal lining, especially when combined with latex. If you notice burning, switch to a plain water‑based lubricant.
How long does it take for the vaginal microbiome to rebalance after stopping the pill?
Typically 4‑6 weeks, but individual timelines vary. Supporting the rebalance with probiotics and avoiding douches speeds up recovery.
What should I do if my copper IUD causes constant spotting?
Spotting is common in the first 3‑6 months. If it continues beyond that, ask your clinician to check the IUD placement. In some cases, a hormonal IUD may be a better fit.
Are there any birth‑control methods that don’t affect vaginal pH?
Non‑hormonal options like copper IUDs, condoms (especially polyurethane), and fertility‑aware methods have minimal impact on pH. However, any device can cause mechanical irritation if not fitted properly.
Understanding how each contraceptive interacts with your body empowers you to choose a method that feels comfortable and safe. Keep track of symptoms, stay in touch with your healthcare provider, and don’t settle for persistent irritation-you deserve a birth‑control option that works without discomfort.