More than 5 million cases of nonmelanoma skin cancer are diagnosed in the U.S. every year. That’s more than all other cancers combined. And the vast majority? Basal cell carcinoma (BCC) and squamous cell carcinoma (SCC). These aren’t rare or obscure - they’re everyday realities for millions of people, especially those over 50 with a history of sun exposure. But here’s the thing most people don’t realize: even though both are called skin cancer, they’re not the same. One grows slowly and rarely spreads. The other? It can move fast - and if ignored, it can become life-threatening.
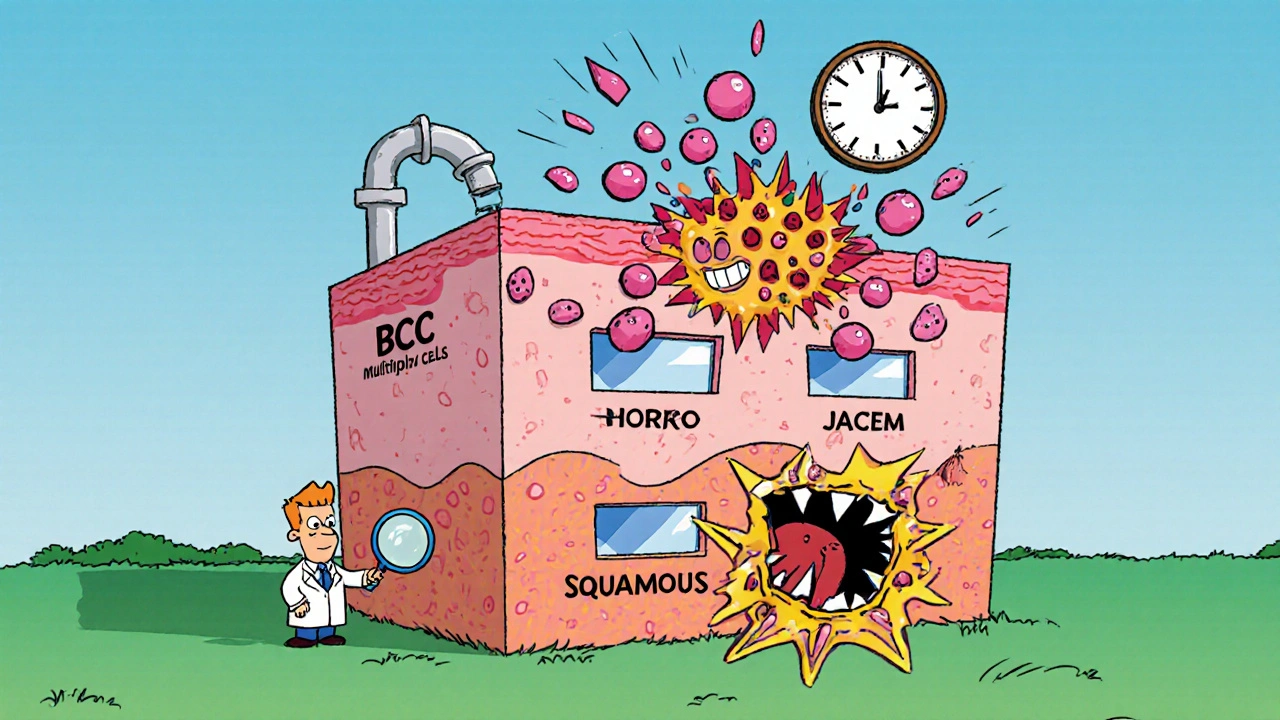
Where They Start: The Skin’s Hidden Layers
Your skin isn’t just one layer. It’s made up of multiple floors, like a building. At the bottom is the basal layer, where new skin cells are born. These cells slowly rise up, flatten out, and become squamous cells by the time they reach the surface. That’s where the names come from.
Basal cell carcinoma starts in that bottom layer. It’s the most common cancer in humans - about 8 out of 10 skin cancers are BCC. Squamous cell carcinoma begins higher up, in the squamous cells. It’s less common, but more dangerous. Think of it this way: BCC is like a leaky faucet - annoying, but usually contained. SCC is more like a burst pipe - it can spread if you don’t shut it off fast enough.
What They Look Like: Spotting the Warning Signs
Both cancers often show up on sun-exposed areas: face, ears, neck, scalp, hands. But their appearances are different.
Basal cell carcinoma usually looks like:
- A shiny, pearly bump - often mistaken for a mole or pimple
- An open sore that bleeds, oozes, or crusts over - and never fully heals
- A scar-like patch that’s flat, white, or yellow - sometimes mistaken for old skin damage
Squamous cell carcinoma typically appears as:
- A firm, red bump - sometimes dome-shaped
- A rough, scaly patch that might be tender or itchy
- A wart-like growth that crusts or bleeds
- An open sore that doesn’t go away - and may get bigger over weeks
One big red flag? If a spot changes fast - growing, bleeding, or becoming painful in just a few weeks - that’s more likely SCC. BCC grows so slowly, you might not notice it for months or even years.
How Fast They Grow: Speed Matters
BCC creeps along at about half a centimeter per year. It’s lazy. It stays put. That’s why many people ignore it - it doesn’t hurt, it doesn’t itch, it just… sits there.
SCC? It’s not patient. It grows 1.5 to 2 centimeters a year - sometimes faster. Aggressive SCCs can double in size in 4 to 6 weeks. That’s not a typo. That’s real. And the faster it grows, the deeper it goes. That’s why SCC often needs bigger surgical cuts to make sure all the cancer is gone.
Metastasis: The Real Difference
This is where things get serious. BCC almost never spreads. Fewer than 0.1% of cases metastasize. That’s like winning the lottery - but in reverse.
SCC? It spreads in 2% to 5% of cases. That’s 20 to 50 times more likely than BCC. And if it spreads? Survival rates drop from 95% to as low as 25%. It doesn’t happen often - but when it does, it’s bad.
Some spots are riskier. SCC on the lip? Up to 14% chance of spreading. On the ear? 9%. On the genital area? 7%. Even a small SCC in one of these areas needs serious attention.
Who Gets It? Age, Skin, and Sun Exposure
Most cases happen after age 50. The average diagnosis age is 67 for both. But there’s a twist: SCC is more common in men. About 65% of SCC patients are male. Why? Probably because of long-term outdoor work - construction, farming, fishing. BCC affects men and women almost equally.
People with fair skin, light eyes, and blonde or red hair are at highest risk. But even darker-skinned people can get it - especially SCC on the legs or in scars. UV exposure is the #1 cause. Not just sunburns. Cumulative exposure over decades matters more for SCC. That’s why daily sunscreen cuts SCC risk by 50%, but only 40% for BCC.
Treatment: What Works and What Doesn’t
Both cancers are highly curable - if caught early. Surgical removal works in over 95% of cases. But the approach differs.
BCC? Often treated with simple excision, cryotherapy (freezing), or even topical creams like imiquimod. For small, shallow BCCs, these work well. Mohs surgery - a precise skin-sparing technique - cures 99% of primary BCCs.
SCC? Needs more aggressive treatment. Topical creams only work about half the time. Mohs surgery still works well - 97% cure rate - but surgeons often need to cut wider margins. That means more tissue removed. More reconstructive surgery. More scarring.
And here’s something most people don’t know: SCC has a higher recurrence rate, especially in people with weak immune systems. Organ transplant patients? They’re 250 times more likely to get SCC than BCC. That’s not a typo. It’s a medical emergency waiting to happen.
What Happens After Treatment
After treatment, follow-up matters. SCC patients need more checkups. On average, they see their dermatologist 2.3 times more often than BCC patients. Why? Because SCC comes back faster - 73% of recurrent SCCs show up within 12 months. For BCC, it’s often 18 months or longer.
Patients with SCC also report more anxiety. On patient forums, 85% of SCC survivors worry about metastasis. Only 42% of BCC patients do. That’s not just fear - it’s based on real risk.
And recovery? SCC patients are more likely to need plastic surgery to fix the damage. About 45% of SCC cases require reconstruction after removal. For BCC, it’s 28%.

New Treatments and What’s Coming
Medicine is catching up. In 2018, the FDA approved the first immunotherapy drug - cemiplimab - for advanced SCC. It works in nearly half of patients who’ve run out of other options. No such drug exists for BCC yet. For advanced BCC, there’s vismodegib - a pill that blocks a specific pathway. It’s effective, but it has serious side effects.
Research is also getting smarter. Scientists now know that 90% of SCCs have a mutation in the TP53 gene - the “guardian of the genome.” Only 50% of BCCs do. That’s why SCC behaves more aggressively. And new AI tools can now analyze skin images with 94% accuracy to tell BCC from SCC - faster than most doctors.
Prevention: The Only Real Shield
You can’t undo sun damage. But you can stop more from happening.
- Wear broad-spectrum SPF 30+ every day - even when it’s cloudy
- Reapply every two hours if you’re outside
- Wear wide-brimmed hats and UV-blocking sunglasses
- Avoid the sun between 10 a.m. and 4 p.m.
- Check your skin monthly - use a mirror for hard-to-see spots
- See a dermatologist yearly - or every 6 months if you’ve had skin cancer before
And if you’ve had one skin cancer? You’re at higher risk for another. One in three people who’ve had BCC or SCC will get another within five years. That’s why prevention isn’t optional - it’s survival.
Final Takeaway: Don’t Wait
Basal cell carcinoma is common. Squamous cell carcinoma is dangerous. But neither is a death sentence - if you catch them early.
That shiny bump? Get it checked. That scaly patch that won’t go away? Don’t ignore it. That sore that bleeds every time you shave? See a doctor.
Most people think skin cancer means melanoma. But melanoma is rare. These two - BCC and SCC - are the real everyday threats. They’re preventable. They’re treatable. But they won’t fix themselves.
Is basal cell carcinoma dangerous?
Basal cell carcinoma is rarely dangerous because it almost never spreads to other parts of the body. But if left untreated, it can grow deep into the skin, damaging nerves, bone, and tissue - especially on the face. While it’s not usually life-threatening, it can cause serious disfigurement and require complex surgery.
Can squamous cell carcinoma spread?
Yes, squamous cell carcinoma can spread - unlike basal cell carcinoma. It metastasizes in about 2-5% of cases, especially when located on the lips, ears, or genital area. Once it spreads, treatment becomes much harder and survival rates drop significantly. Early detection is critical.
Which is more common: BCC or SCC?
Basal cell carcinoma is far more common, making up about 80% of all nonmelanoma skin cancers. Squamous cell carcinoma accounts for roughly 20%. BCC is the most common cancer in humans overall.
Do I need a biopsy to confirm skin cancer?
Yes. A biopsy - where a small sample of the suspicious skin is removed and examined under a microscope - is the only way to confirm whether it’s BCC, SCC, or something else. Visual inspection alone isn’t enough, even for experienced dermatologists.
Can I treat skin cancer with over-the-counter creams?
Only in very specific cases. Topical creams like imiquimod or 5-fluorouracil may work for very early, superficial basal cell carcinomas. But they’re ineffective for most squamous cell carcinomas and not recommended for deeper or aggressive lesions. Always consult a dermatologist - self-treatment can delay proper care.
How often should I get my skin checked?
If you’ve never had skin cancer, an annual checkup is enough. If you’ve had BCC or SCC, you should see a dermatologist every 6 to 12 months. People with a history of multiple skin cancers or weakened immune systems may need checkups every 3 to 6 months.
What Comes Next?
If you’ve been diagnosed with either BCC or SCC, your next step is simple: follow your doctor’s plan. Don’t delay treatment. Don’t assume it’s “just a spot.” And don’t stop protecting your skin.
If you haven’t been diagnosed yet - but you’ve noticed something odd - don’t wait. Make that appointment. Skin cancer doesn’t care if you’re busy, scared, or think it’ll go away. It just grows. And the earlier you catch it, the easier it is to fix.