Betamethasone Usage Safety Calculator
Enter your application details below to determine safe usage duration and potential risk level. Based on the article's guidance: Never use for more than 2-4 weeks on face or 4-6 weeks on body without medical supervision.
Results
Ever wonder why a prescription cream can make your skin look smoother overnight, yet you hear warnings about thinning it out? The answer lies in how Betamethasone is a potent synthetic corticosteroid used on the skin to reduce inflammation and modulate cellular turnover. This article breaks down exactly what happens at the microscopic level when you slap a betamethasone‑based product on your skin, how it influences exfoliation, and what that means for long‑term renewal.
What betamethasone does to the skin’s architecture
Betamethasone belongs to the class of Corticosteroids drugs that mimic the hormone cortisol and affect inflammation, immune response, and cell growth. When applied topically, it penetrates the stratum corneum and reaches the Epidermis the outermost skin layer composed of several sub‑layers of keratinocytes. Inside the epidermis, the drug binds to glucocorticoid receptors, triggering a cascade that dampens inflammatory cytokines and slows the proliferation of Keratinocytes the primary cells that produce keratin and form the bulk of the epidermal barrier.
Because keratinocyte turnover is a core driver of natural exfoliation, any drug that tampers with their division directly changes how quickly dead skin cells are shed. In simple terms, betamethasone tells the skin to ‘take a breather,’ which can both calm red, inflamed lesions and temporarily reduce the shedding rate.
Why the skin may feel smoother - the short‑term effect
Within days of using a betamethasone cream, two things happen:
- Inflammation subsides, so the usual swelling and fluid that mask the skin’s true texture disappear.
- Edema (water‑logged tissue) resolves, allowing the epidermis to flatten and appear less “puffy.”
This dual action creates the illusion of smoother skin, even though the underlying exfoliation process might be slowing down. The skin looks calmer, not necessarily more regenerated.
Long‑term renewal: thinning vs. strengthening
Extended use (more than two weeks) raises a different set of concerns. Betamethasone’s anti‑proliferative effect can lead to epidermal thinning. A thinner epidermis means the natural barrier is weaker, making it easier for irritants and microbes to slip through. Over time, the reduction in cell turnover translates to less frequent shedding of dead cells, which may manifest as:
- Dull, uneven skin tone
- Increased susceptibility to contact dermatitis
- Visible blood vessels (telangiectasia) because the skin offers less camouflage
However, there’s a flip side. By controlling chronic inflammation in conditions like Psoriasis an autoimmune disease characterized by rapid skin cell buildup and thick plaques, betamethasone can actually reset the renewal cycle. When the hyper‑proliferative flare calms, the skin resumes a more normal, balanced turnover, which eventually leads to healthier renewal patterns-provided the steroid is tapered correctly.
Comparing betamethasone with other topical agents
Not all skin‑active compounds work the same way. Below is a quick snapshot that helps you see where betamethasone sits relative to two common alternatives.
| Agent | Potency (class) | Effect on keratinocyte turnover | Typical use case |
|---|---|---|---|
| Betamethasone | High (class I) | ↓ proliferation → slower exfoliation (short‑term smoothness, long‑term thinning) | Severe eczema, psoriasis plaques |
| Hydrocortisone | Low (class VII) | Minor ↓ proliferation → minimal impact on shedding | Mild dermatitis, irritant rash |
| Retinoids (e.g., tretinoin) | Non‑steroidal | ↑ proliferation → faster exfoliation and collagen remodeling | Acne, photo‑aging, skin texture improvement |
Notice how retinoids push the opposite direction-speeding up turnover for renewal-while betamethasone primarily slows it down to calm inflammation.
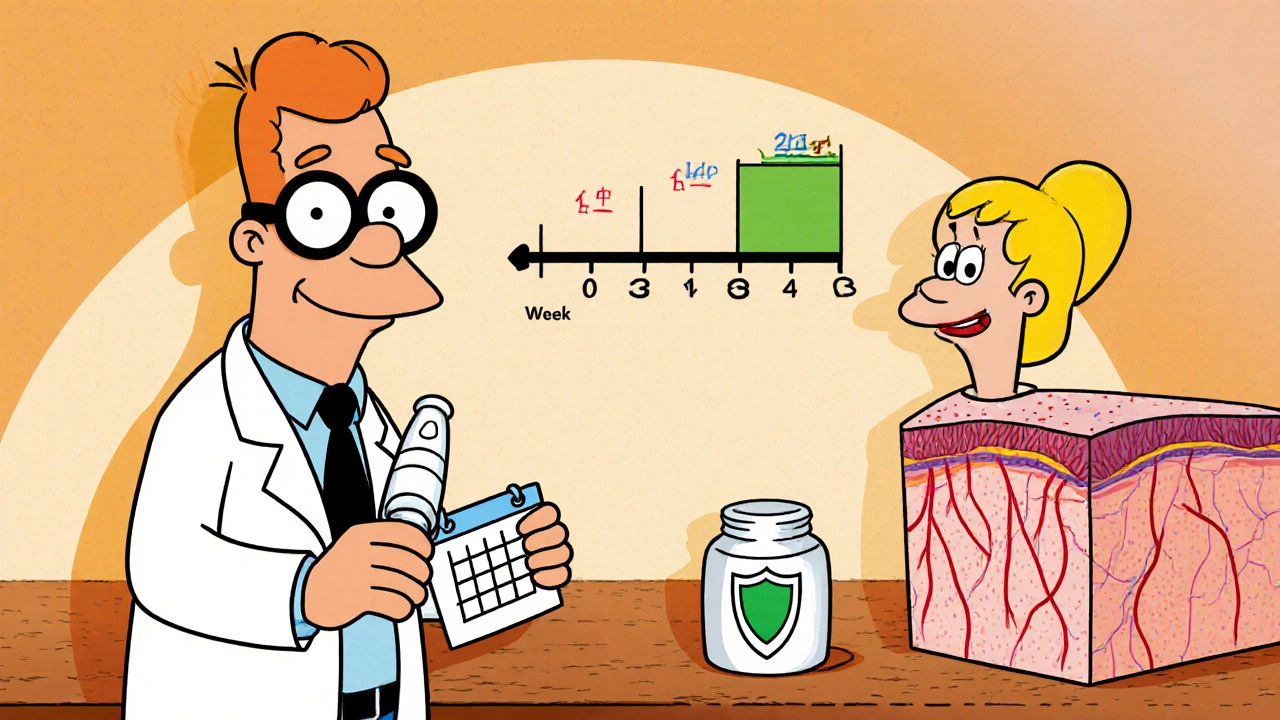
Practical tips for using betamethasone without sacrificing renewal
If you’ve been prescribed betamethasone, follow these proven steps to keep your skin’s natural renewal humming:
- Limit duration: Use the cream for no longer than 2-4 weeks unless a dermatologist says otherwise.
- Pick the right strength: For facial areas, opt for a lower‑potency formulation (often 0.05% or less).
- Apply thinly: A pea‑size amount for a typical adult’s face is enough; over‑application increases thinning risk.
- Moisturize after: A fragrance‑free barrier cream restores lipids lost during steroid use.
- Taper off: Gradually reduce frequency (e.g., daily → every other day → twice a week) to give keratinocytes a chance to resume normal turnover.
- Combine with gentle exfoliants: Low‑strength AHAs or enzymatic peels on non‑treated days can keep the skin surface fresh without provoking irritation.
When to seek professional advice
Even with careful use, certain signs signal it’s time to call a dermatologist:
- Visible thinning or sparkle‑like translucency of skin
- Persistent redness or a rash that spreads beyond the original area
- Development of stretch marks (striae) on the face, arms, or thighs
- Worsening of the original condition despite treatment
These symptoms often mean the steroid is doing more harm than good, and a switch to a milder agent or a non‑steroidal option may be warranted.
Bottom line: betamethasone balances calm with caution
In a nutshell, betamethasone is a double‑edged sword. It excels at dialing down inflammation, which instantly makes skin look smoother. The trade‑off is a slowdown in natural exfoliation that, if left unchecked, can thin the epidermis and impair long‑term renewal. By respecting treatment duration, potency, and follow‑up skin‑care, you can harvest the anti‑inflammatory benefits while keeping your skin’s renewal engine humming.
How quickly does betamethasone start affecting skin turnover?
Most patients notice a reduction in visible inflammation within 48‑72 hours, but measurable changes in keratinocyte proliferation usually appear after about a week of consistent use.
Can I use betamethasone on acne‑prone skin?
It’s generally not recommended because the steroid can mask acne lesions while still thinning the skin, which may exacerbate breakouts once you stop using it.
Is there a safe way to combine betamethasone with retinoids?
Only under dermatologist guidance. Usually, the two are alternated (steroid nights, retinoid mornings) with ample moisturization to prevent barrier breakdown.
What signs indicate my skin barrier is compromised?
Persistent tightness, stinging, visible peeling, or a shiny translucent appearance are classic red flags that the barrier needs repair.
How do I transition off betamethasone after a flare?
Gradually reduce frequency over 1-2 weeks while introducing a gentle, non‑comedogenic moisturizer. If the condition re‑emerges, switch to a lower‑potency steroid or a non‑steroidal anti‑inflammatory.




