Most people drink coffee without thinking twice. But if you're taking any kind of medication, that morning cup might be doing more than just waking you up-it could be making your drugs less effective, or even dangerous.
Why Caffeine Isn't Just a Morning Pick-Me-Up
Caffeine isn’t just a stimulant. It’s a powerful chemical that interacts with your body’s drug-processing systems. It blocks adenosine receptors to keep you alert, but it also messes with enzymes in your liver-specifically CYP1A2-that break down about 10% of all prescription and over-the-counter medications. That means when you drink coffee, energy drinks, or even tea, you’re not just consuming caffeine. You’re changing how your body handles other drugs.For most healthy adults, up to 400 mg of caffeine a day (roughly four cups of coffee) is considered safe. But if you’re on medication, that number can drop fast. Your metabolism, liver function, age, and even your genes affect how your body handles caffeine. Some people break it down in an hour. Others take nearly 10 hours. And if you have liver disease, that time can stretch to four full days.
Levothyroxine and Coffee: A Silent Threat to Thyroid Health
If you take levothyroxine for hypothyroidism, drinking coffee with your pill could be sabotaging your treatment. Research shows that caffeine in coffee reduces the absorption of levothyroxine by up to 55%. That means your body isn’t getting the full dose-even if you take it exactly as prescribed.One patient, who posted under the username 'ThyroidWarrior2023' on Reddit, saw their TSH level jump from 1.8 to 8.7 after taking levothyroxine with coffee for three weeks. Their endocrinologist confirmed it was textbook interference. TSH levels that high mean your thyroid isn’t working properly, and you could be at risk for fatigue, weight gain, depression, and heart problems.
The American Thyroid Association’s 2023 guidelines are clear: wait at least 60 minutes after taking levothyroxine before drinking coffee. Some doctors recommend waiting up to 90 minutes for maximum absorption. And don’t think switching to decaf helps-it still contains enough caffeine to interfere. Even black tea can cause the same issue.
Warfarin and Caffeine: The Hidden Bleeding Risk
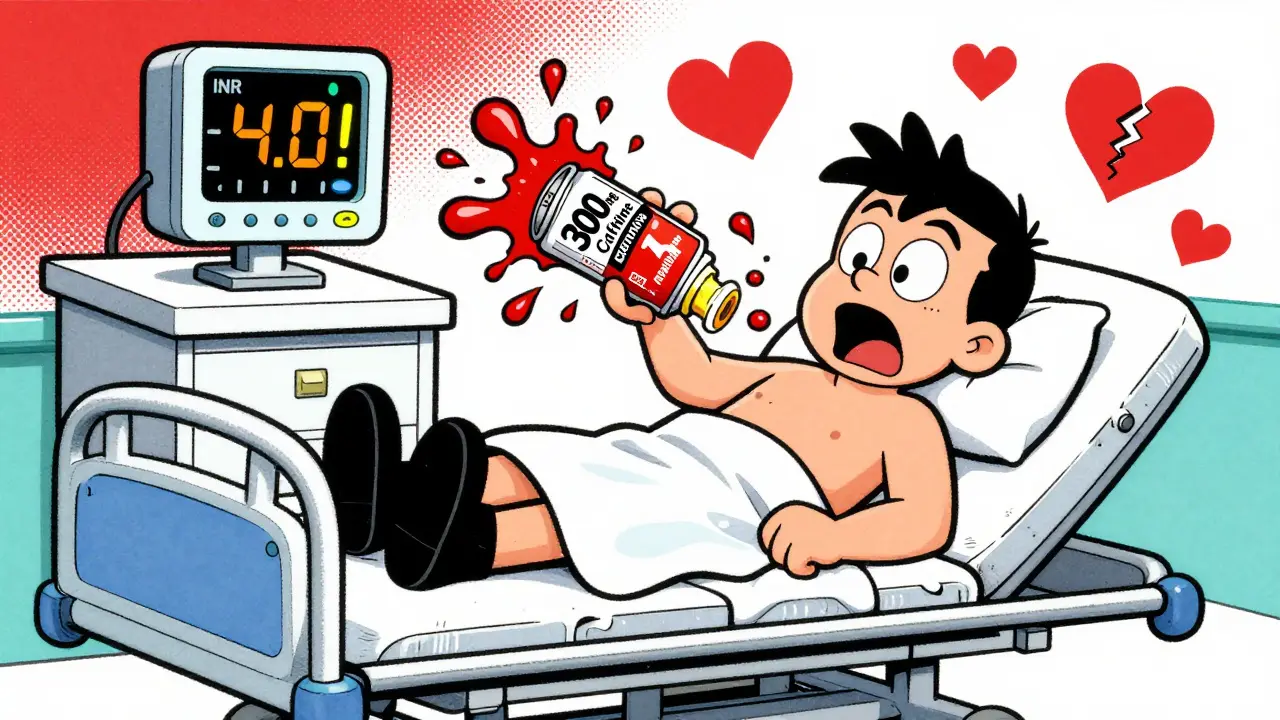
Warfarin is a blood thinner used to prevent clots, strokes, and heart attacks. It’s one of the most commonly prescribed drugs in the UK and US. But it’s also one of the most sensitive to caffeine.Caffeine blocks the CYP1A2 enzyme that breaks down warfarin. When that happens, warfarin builds up in your blood. That increases your INR-the measure of how long it takes your blood to clot. A normal INR is between 2 and 3 for most patients. But with caffeine, it can spike to 4 or higher. That puts you at serious risk of bleeding: nosebleeds, bruising, internal bleeding, even strokes caused by bleeding in the brain.
According to a University of Michigan survey from January 2024, 41% of warfarin users who drank more than 200 mg of caffeine daily (about two strong coffees) had unexplained INR spikes above 4.0. Nearly one in five of those patients ended up in the emergency room because of bleeding.
The FDA’s warfarin prescribing guidelines (updated January 2024) warn: don’t suddenly increase your caffeine intake. If you normally drink one cup of coffee a day, keep it that way. Don’t start drinking three. Don’t switch to energy drinks. Even small changes can throw your INR out of balance.
Heart Medications: Caffeine Can Cancel Out Your Treatment
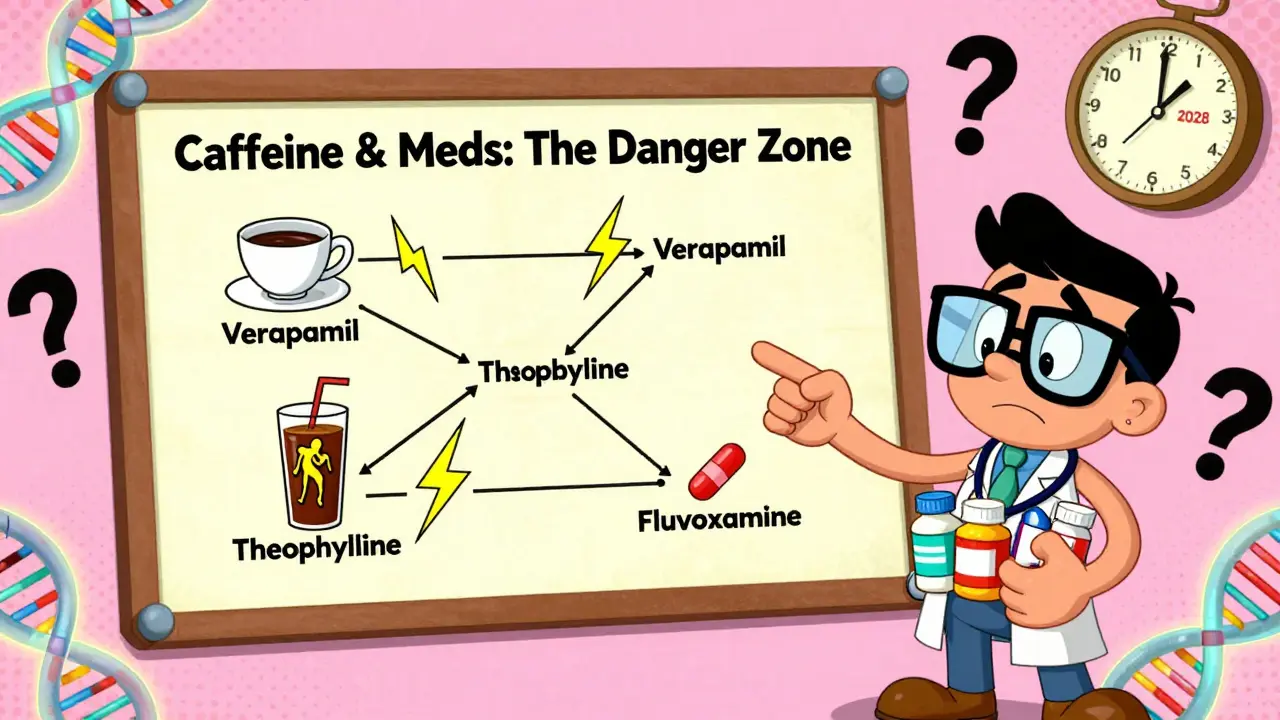
If you’re on medications for high blood pressure or heart rhythm problems, caffeine might be working against you.Verapamil, a calcium channel blocker used to treat high blood pressure and arrhythmias, loses 25-30% of its effectiveness when taken with coffee. That’s not a small drop-it’s enough to let your blood pressure creep back up, or your heart to race again. Harvard Health says the best fix is to wait at least two hours after taking verapamil before having coffee.
Even more alarming: adenosine and dipyridamole, drugs used in cardiac stress tests, become nearly useless if you’ve had caffeine in the past 24 hours. These drugs are used to simulate exercise on your heart so doctors can spot blockages. But caffeine blocks the same receptors they target. In clinical studies, caffeine reduced their effectiveness by 70-90%. That means your test could come back normal when it shouldn’t-delaying diagnosis of a serious heart problem.
Doctors now routinely ask patients: “Did you have coffee, tea, or energy drinks in the last 24 hours?” If you say yes, they’ll reschedule your test. Don’t risk it.
Antidepressants, Asthma Drugs, and the Hidden Danger of Synergy
Caffeine doesn’t just interfere with absorption-it can amplify side effects.Some SSRIs, like fluvoxamine, are metabolized by the same liver enzyme as caffeine. When you take them together, your body can’t clear either one properly. Harvard Health found that caffeine reduces SSRI absorption by about 33%. That means your depression or anxiety treatment might not work as well. Users on Drugs.com report increased anxiety, jitteriness, and insomnia when combining caffeine with SSRIs.
And then there’s theophylline, an older asthma medication. It’s chemically very similar to caffeine. Both are metabolized by CYP1A2. When you take them together, caffeine can push theophylline levels up by 15-20%. That might sound small, but theophylline has a narrow safety window. Too much can cause nausea, rapid heartbeat, tremors, or even seizures. The University Hospitals 2025 guidelines say asthma patients on theophylline should limit caffeine to under 100 mg per day-about one small coffee-and watch for heart rates over 100 bpm.
Even over-the-counter cold meds can be risky. Pseudoephedrine, found in many decongestants, raises heart rate and blood pressure. Caffeine does the same. Together, they can spike your heart rate by 20-30 beats per minute. That’s dangerous if you have heart disease or high blood pressure.
Energy Drinks Are the Real Problem
Coffee is one thing. Energy drinks are another.They don’t just contain more caffeine-some have 300 mg per can. That’s more than three cups of coffee. But they also add taurine, ginseng, guarana, sugar, and other stimulants that can independently affect drug metabolism. The FDA reports that energy drinks account for 68% of serious caffeine-drug interaction cases.
A 2021 study found that people on five or more daily medications had 3.2 times higher risk of dangerous interactions with caffeine. That’s not a coincidence. If you’re managing diabetes, heart disease, depression, or thyroid issues, you’re likely on multiple drugs. Each one adds another layer of risk.
And here’s the kicker: most people don’t know this is happening. A JAMA Internal Medicine study from April 2024 found that 62% of patients had no idea caffeine could interfere with their meds-even though 89% drank it daily.
What You Should Do Right Now
If you take any prescription or over-the-counter medication, here’s what to do:- Check your meds. Look at the label or ask your pharmacist: does it say anything about caffeine or coffee?
- Know your dose. A cup of coffee has 95-200 mg of caffeine. A can of energy drink can have 80-300 mg. Track your daily intake.
- Time it right. For levothyroxine: wait 60-90 minutes. For verapamil: wait 2 hours. For warfarin: keep your caffeine intake consistent-no sudden spikes.
- Watch for symptoms. If your medication seems less effective, or you feel jittery, anxious, or your heart races, caffeine might be the cause.
- Talk to your pharmacist. Pharmacists are trained to catch these interactions. Ask them: “Does my medication interact with caffeine?”
There’s no need to quit coffee entirely. But if you’re on medication, you need to treat caffeine like a drug-because it is one.
What’s Changing in 2025 and Beyond
Healthcare is catching up. The European Medicines Agency updated its guidelines in March 2025 to include specific warnings for new anticoagulants like edoxaban. The NIH launched a $4.7 million study in January 2025 to see how genetic differences affect caffeine-drug interactions. Epic Systems, one of the largest electronic health record providers, rolled out a pilot program in 47 hospitals that flags caffeine-medication risks automatically-and it’s already cut adverse events by 29%.By 2028, personalized caffeine guidance based on genetic testing could become standard. But you don’t need to wait for that. Right now, you have the power to protect yourself. Just ask the simple question: “Could my coffee be making my medicine less safe?”
Can I drink coffee while taking levothyroxine?
It’s not recommended to drink coffee at the same time as levothyroxine. Coffee can reduce absorption of the medication by up to 55%. Wait at least 60 minutes after taking your pill before having coffee. Even decaf coffee contains enough caffeine to interfere, so avoid it entirely during this window.
Does caffeine affect blood thinners like warfarin?
Yes. Caffeine inhibits the enzyme that breaks down warfarin, causing it to build up in your blood. This raises your INR level, increasing your risk of bleeding. Even small increases in caffeine intake-like switching from one to three cups of coffee a day-can cause dangerous spikes. Keep your caffeine intake consistent and avoid energy drinks, pre-workout supplements, or large amounts of tea.
Can caffeine make my antidepressants less effective?
For some antidepressants, yes. Fluvoxamine and other SSRIs are affected by caffeine because they share the same liver enzyme pathway. Studies show caffeine can reduce SSRI absorption by about 33%, which may lower their effectiveness. Users often report increased anxiety, restlessness, or insomnia. If your symptoms worsen after starting coffee, talk to your doctor about timing or reducing intake.
Are energy drinks more dangerous than coffee with medication?
Yes. Energy drinks often contain 80-300 mg of caffeine per serving-more than coffee-and include other stimulants like taurine, ginseng, and guarana. These ingredients can independently affect drug metabolism and increase side effects. The FDA reports that 68% of serious caffeine-medication interactions involve energy drinks. Avoid them entirely if you’re on any medication.
Should I stop drinking coffee altogether if I’m on medication?
Not necessarily. You don’t need to quit coffee unless your doctor advises it. The key is consistency and timing. If you’re on levothyroxine, wait an hour. If you’re on warfarin, keep your intake steady. If you’re on heart or asthma meds, check with your pharmacist. Small changes in timing or amount can prevent serious problems without giving up your daily ritual.