Drug Causality Assessment Tool
Assess Drug Causality
Determine the probability that a medication caused an adverse reaction using dechallenge and rechallenge evidence.
Assessment Results
Probability Score
0% probability of drug causality
Key Factors
- Dechallenge Evidence 0
- Rechallenge Evidence 0
- Onset Timing 0
Interpretation
Important Notes
This tool provides an assessment based on clinical principles but does not replace professional medical judgment. Rechallenge should only be done under strict medical supervision when absolutely necessary. Always consult with a healthcare provider for patient care decisions.
When a patient starts a new medication and suddenly develops a rash, dizziness, or liver problems, doctors face a tough question: Is this drug causing the problem? It’s not always obvious. Many symptoms overlap with other illnesses, and patients often take multiple drugs. That’s where dechallenge and rechallenge come in-two simple but powerful clinical tools used to figure out if a drug is truly responsible for an adverse reaction.
What Is Dechallenge?
Dechallenge means stopping the suspected drug and watching what happens. If the side effect gets better-or disappears-after the drug is stopped, that’s called a positive dechallenge. It’s a strong hint that the drug was the culprit. For example, a patient on metronidazole for a bacterial infection develops a painful, recurring rash on their ankles. The doctor stops the drug. Within five days, the rash fades. The skin doesn’t turn red anymore. The itching stops. That’s a positive dechallenge. It doesn’t prove the drug caused it, but it makes the link much more likely. A negative dechallenge means the symptoms didn’t improve after stopping the drug. That suggests something else is going on-maybe an unrelated infection, an autoimmune issue, or another medication. Sometimes, damage is permanent. If a drug caused liver failure and the patient still has high enzyme levels weeks after stopping it, that’s a negative dechallenge because the harm didn’t reverse. Dechallenge is the first step in almost every case. It’s safe, non-invasive, and often required by law. Regulatory agencies like the FDA and EMA expect this step to be documented in every adverse drug reaction report.What Is Rechallenge?
Rechallenge is when the drug is given again-on purpose-to see if the same reaction comes back. If the rash, nausea, or dizziness returns exactly as before, that’s a positive rechallenge. And this is the gold standard. In the same metronidazole case, after the rash cleared, the patient was given the drug again under close medical supervision. Within 48 hours, the exact same rash reappeared on the same spot on the ankle. That’s not coincidence. That’s proof. Rechallenge is rare, and for good reason. Giving a drug back to someone who had a serious reaction is risky. If the reaction was Stevens-Johnson Syndrome, toxic epidermal necrolysis, or drug-induced liver failure, rechallenge could kill the patient. So it’s only done in very specific situations: mild reactions, when the drug is essential, and only with full informed consent and emergency support ready. According to data from the World Health Organization, a positive rechallenge raises the likelihood that a drug caused the reaction from “probable” to “definite” in 97% of cases. No algorithm, no lab test, no statistical model comes close to that level of certainty.Why These Tests Matter in Real Life
Imagine a 68-year-old woman with arthritis who starts taking a new NSAID. Two weeks later, she develops severe nausea and vomiting. Her doctor assumes it’s a stomach bug. She’s prescribed anti-nausea meds. The vomiting continues. A month later, she’s hospitalized with dehydration. If the doctor had done a dechallenge-stopped the NSAID and waited three days-the vomiting might have stopped. That would have pointed to the drug. But without that step, she’s stuck on a medication that’s making her sick, and the real cause stays hidden. In dermatology, dechallenge is used in 87% of suspected drug rash cases. In liver injury, it’s used in 79%. But in psychiatry, where stopping antidepressants can trigger suicidal thoughts, dechallenge is used in only 43% of cases. That’s not because doctors don’t care-it’s because the risk of stopping the drug is too high. That’s why dechallenge is the workhorse of pharmacovigilance. Rechallenge is the rare, high-stakes confirmation.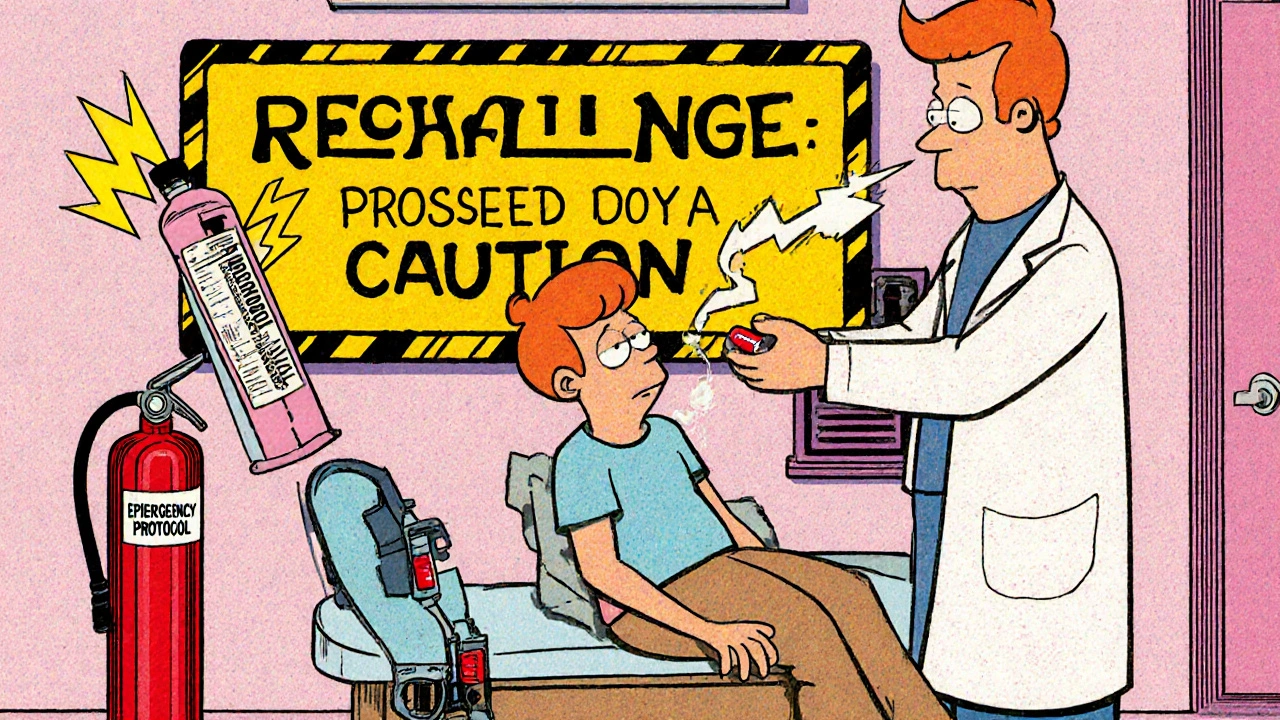
How Doctors Use These Tools in Practice
Dechallenge isn’t just “stop the drug and hope.” It’s systematic.- The doctor notes exactly when the side effect started and how severe it was.
- The drug is stopped, and the patient is monitored for 5 to 14 days, depending on the drug’s half-life.
- Other possible causes are ruled out: infections, new foods, other medications, stress.
- Improvement is documented with photos, lab results, or symptom scores.
- Only done under supervision in a clinic or hospital.
- Requires approval from an ethics board or institutional review committee.
- Patient signs detailed consent forms explaining the risks.
- Emergency meds and staff are on standby.
- The drug is given in a low dose first, then gradually increased if no reaction occurs.
Why Rechallenge Is So Rare (and Why That’s Okay)
Only 0.3% of serious adverse drug reaction cases involve rechallenge. Why? Because the risk is too high. A patient who had a life-threatening skin reaction to a painkiller? No doctor will give it back. A patient who had a mild, itchy rash? Maybe. Especially if that drug is the only one that controls their condition. There’s also a practical problem: time. If the reaction happened six months ago, the patient may have switched to another drug, forgotten the details, or moved away. Rechallenge becomes impossible. And polypharmacy makes it messy. If a patient is on 10 medications and one causes a rash, stopping all of them at once won’t tell you which one was responsible. That’s why doctors need clear timelines-when each drug was started, stopped, or changed.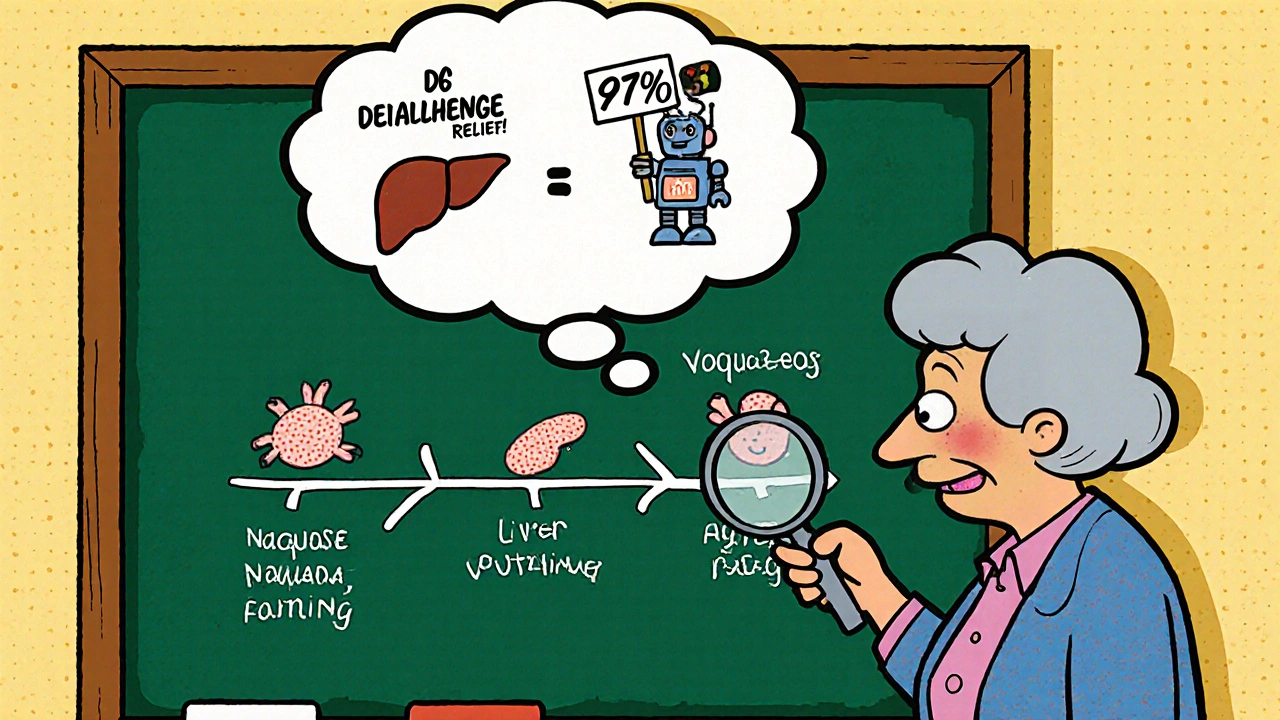
What’s New in Dechallenge and Rechallenge?
Technology is helping-but not replacing-these classic methods. Wearable sensors can now track heart rate, skin temperature, and activity levels automatically after a drug is stopped. If a rash is fading, the patient’s sleep improves, and their movement increases, that’s objective proof of dechallenge-no more relying on the patient’s memory. Researchers are also developing blood tests that check for immune cell reactions to specific drugs. In lab tests, these can predict whether someone will react to a drug with 89% accuracy. That could one day replace rechallenge entirely. But here’s the catch: no algorithm can replicate the real-world experience of a patient’s body reacting to a drug. As one WHO expert put it: “No algorithm can substitute for the clinical reality of symptom resolution after drug discontinuation.”What This Means for Patients
If you’ve had a strange reaction to a medication, don’t ignore it. Write down:- What drug you took
- When you started it
- When the symptom started
- What happened when you stopped it
- Any changes in how you felt
Bottom Line
Dechallenge is the everyday tool. Rechallenge is the rare, powerful confirmation. Together, they turn suspicion into certainty. In a world full of drugs, side effects, and uncertainty, these two steps are among the most reliable ways to find out what’s really causing harm. They’re simple. They’re low-tech. And they’ve saved countless lives.Even with all the fancy AI and genetic tests coming out, nothing beats watching a patient’s symptoms vanish after stopping a drug-and knowing exactly why.
What is a positive dechallenge?
A positive dechallenge happens when an adverse reaction improves or disappears after stopping the suspected drug. This suggests the drug was likely the cause. For example, if a rash fades within days after discontinuing a medication, that’s a positive dechallenge.
Can rechallenge be dangerous?
Yes, rechallenge can be dangerous, especially for severe reactions like Stevens-Johnson Syndrome, liver failure, or anaphylaxis. It’s only done in rare cases under strict medical supervision with emergency plans in place. For life-threatening reactions, rechallenge is almost never performed.
Why isn’t rechallenge used more often?
Rechallenge is avoided because it risks repeating a harmful reaction. Ethical guidelines and regulatory agencies limit it to non-life-threatening cases where the benefit of confirming drug causality outweighs the risk. Less than 0.3% of serious adverse reaction cases involve rechallenge.
How do doctors know if a reaction is caused by a drug?
Doctors use four key factors: timing (did the reaction start soon after taking the drug?), dechallenge (did symptoms improve after stopping?), rechallenge (did symptoms return when the drug was given again?), and biological plausibility (is the reaction known to be linked to the drug?). Dechallenge and rechallenge provide the strongest clinical evidence.
Are there alternatives to rechallenge?
Yes. Blood tests that measure immune cell responses to drugs are being developed and can predict reactions with up to 89% accuracy. Wearable sensors can track symptom resolution after dechallenge. But these tools are still being validated. Clinical dechallenge remains the gold standard for confirming causality.