When you're managing type 2 diabetes, finding a medication that lowers blood sugar without causing low blood sugar or weight gain feels like a win. That’s why SGLT2 inhibitors became so popular. Drugs like canagliflozin, dapagliflozin, and empagliflozin don’t just help control glucose-they also cut heart failure risks and protect your kidneys. But there’s a hidden side effect that catches many people off guard: yeast infections and serious urinary problems.
How SGLT2 Inhibitors Work-and Why They Cause Infections
SGLT2 inhibitors work by making your kidneys dump extra sugar into your urine. Normally, your kidneys reabsorb glucose back into your blood. These drugs block that process, so 40 to 110 grams of sugar end up in your urine every day. That sounds like a good thing-until you realize sugar in urine is like pouring honey into a petri dish.
Yeast, especially Candida, thrives in sugary environments. For women, this means vulvovaginal candidiasis-itching, burning, thick white discharge. For men, it’s balanitis: redness, swelling, and pain around the head of the penis. These aren’t rare. Around 3% to 5% of people on these drugs get genital yeast infections, compared to just 1% to 2% on placebos or other diabetes meds.
It’s not just the genitals. The sugar in your urine also raises the risk of urinary tract infections (UTIs). Bacteria like E. coli love that sweet, warm environment. Studies show SGLT2 inhibitors increase your risk of UTIs by nearly 80% compared to other diabetes drugs like DPP-4 inhibitors or sulfonylureas. And while most UTIs are mild, some turn dangerous fast.
The Real Danger: When a UTI Turns Life-Threatening
Most people think of a UTI as a burning sensation and frequent peeing. But with SGLT2 inhibitors, things can escalate quickly. In 2015, the FDA reviewed data from over 19,000 patients and found 19 cases of urosepsis-blood poisoning from a kidney infection-linked to these drugs. Ten of those were from canagliflozin, nine from dapagliflozin. Four patients ended up in intensive care. Two needed dialysis because their kidneys failed.
One case from the National Institutes of Health tells the whole story. A 64-year-old woman with no prior infection history started dapagliflozin. Within six weeks, she developed emphysematous pyelonephritis-a rare, gas-forming kidney infection that can destroy tissue. She needed two surgeries, 14 days of IV antibiotics, and nearly died. Eleven months later, after restarting the drug, the infection came back-this time with a perinephric abscess.
Even rarer but deadlier is Fournier’s gangrene, a necrotizing infection of the genitals and perineum. It’s seen in fewer than 1 in 1,000 users, but it kills fast. The European Medicines Agency added it to warning labels in 2016. Symptoms? Severe pain, swelling, redness, fever, or a foul smell from the genital area. If you have any of these, don’t wait. Go to the ER.
Who’s Most at Risk?
Not everyone on SGLT2 inhibitors gets infections. But some people are far more vulnerable:
- Women (due to shorter urethras and natural yeast presence)
- People over 65
- Those with a history of recurrent UTIs or yeast infections
- People with poor hygiene or urinary retention
- Those with kidney disease (eGFR below 60)
- Patients with HbA1c above 8.5%
A 2024 study in Diabetes Care created a simple 5-point risk score. If you score 3 or higher, your chance of a serious urinary infection jumps to over 15%. That’s not a small risk-it’s a red flag.
Doctors in Birmingham, like those at the Queen Elizabeth Hospital, now screen for these factors before prescribing. If you’ve had three UTIs in the past year, they’ll likely skip SGLT2 inhibitors and go for a GLP-1 agonist or DPP-4 inhibitor instead.

How These Drugs Compare to Other Diabetes Treatments
It’s not fair to judge SGLT2 inhibitors in isolation. You have to weigh the benefits against the risks.
Compared to sulfonylureas-which cause low blood sugar and weight gain-SGLT2 inhibitors are safer for your heart and much better for your waistline. Compared to metformin, they don’t cause stomach upset. And compared to insulin, they don’t require injections or constant blood sugar checks.
But when it comes to infections? No other major diabetes drug does this. DPP-4 inhibitors, GLP-1 agonists, and metformin don’t dump sugar into your urine. Their infection rates are close to placebo levels. So if you’re prone to UTIs or yeast, switching to one of these might be smarter.
Here’s a quick comparison:
| Medication Class | Genital Yeast Infection Risk | UTI Risk | Cardiovascular Benefit |
|---|---|---|---|
| SGLT2 Inhibitors | 3-5% | 1.7x higher than comparators | Yes (proven) |
| DPP-4 Inhibitors | 1-2% | Similar to placebo | No |
| GLP-1 Agonists | 1-2% | Similar to placebo | Yes (strong) |
| Sulfonylureas | 1-2% | Similar to placebo | No |
| Metformin | 1-2% | Similar to placebo | Mild |
So if you’re young, healthy, and have heart disease or kidney disease, SGLT2 inhibitors might be your best bet. But if you’ve had even one yeast infection before, or you’re a woman over 60 with a history of UTIs, the risk may not be worth it.
What You Can Do to Lower Your Risk
If your doctor says SGLT2 inhibitors are right for you, don’t panic. There are real steps you can take to protect yourself:
- Wipe front to back after using the toilet-this stops bacteria from entering the urethra.
- Drink more water. At least 1.5 to 2 liters a day. Flushes out sugar and bacteria.
- Urinate after sex. Reduces bacterial buildup.
- Wear cotton underwear and avoid tight pants. Moisture traps yeast.
- Don’t use scented soaps or douches. They upset your natural balance.
- Consider cranberry products. A 2023 FDA safety update noted that daily cranberry supplements reduced UTIs by 29% in SGLT2 users. It’s not a cure, but it helps.
And if you notice any of these symptoms, call your doctor immediately:
- Itching, burning, or redness in the genital area
- Pain or pressure in your lower back or sides
- Fever above 100.4°F
- Cloudy, bloody, or foul-smelling urine
- Swelling or tenderness from your genitals to your rectum
Don’t wait for it to get worse. SGLT2-related infections can turn from mild to critical in 48 hours.
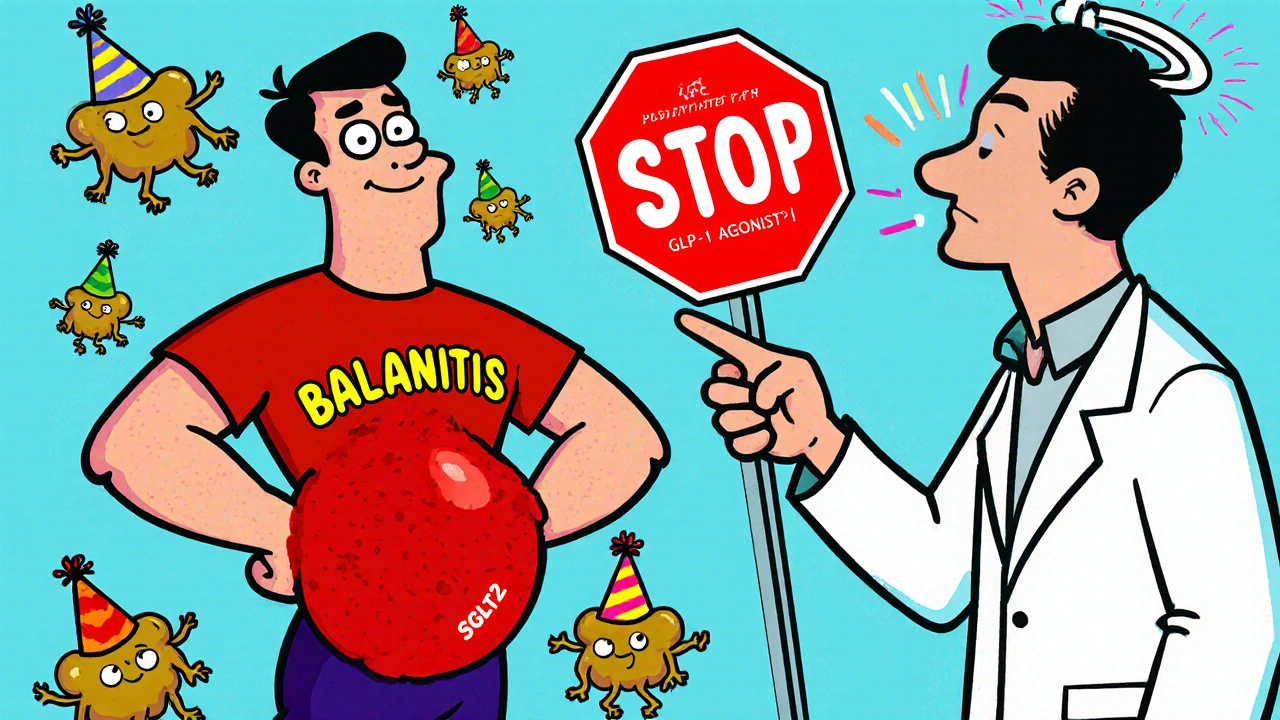
When to Stop or Switch
One in four patients on SGLT2 inhibitors stops taking them within two years-mostly because of infections. That’s a lot. If you’ve had two or more yeast infections or UTIs while on the drug, it’s time to talk about alternatives.
GLP-1 agonists like semaglutide (Ozempic, Wegovy) or liraglutide (Victoza) are now preferred for patients with heart disease or obesity who need strong glucose control without infection risks. DPP-4 inhibitors like sitagliptin are gentler on the urinary tract and work well with metformin.
The American Diabetes Association updated its guidelines in 2023 to say: "Avoid SGLT2 inhibitors in patients with recurrent UTIs or genital infections." That’s not a suggestion-it’s a rule.
Final Thoughts: Benefits vs. Real Risks
SGLT2 inhibitors are powerful. They save lives. They reduce heart attacks, strokes, and kidney failure. But they’re not magic pills. They come with a price: your urinary tract.
For someone with heart failure and no prior infections? The benefits far outweigh the risks. For a woman in her 70s who’s had three UTIs in the last year? The risk is too high.
It’s not about avoiding these drugs altogether. It’s about using them wisely. Know your body. Know your history. And if you’re on one, pay attention to what your body tells you. A little itching or discomfort isn’t normal. It’s a signal.
Diabetes treatment isn’t one-size-fits-all. The right drug for you isn’t the one with the most buzz-it’s the one that keeps you healthy without putting you in the hospital.
Can SGLT2 inhibitors cause yeast infections in men?
Yes. While yeast infections are more common in women, men taking SGLT2 inhibitors can develop balanitis-an inflammation of the head of the penis. Symptoms include redness, swelling, itching, and sometimes a thick, white discharge. It’s not rare: studies show men on these drugs have up to 4 times the risk compared to those on other diabetes medications. Good hygiene and staying hydrated can help reduce the chance.
Are SGLT2 inhibitors still safe to take if I have a history of UTIs?
Generally, no. If you’ve had two or more urinary tract infections in the past year, doctors are advised to avoid SGLT2 inhibitors. The risk of recurrence-and possible progression to a severe kidney infection-is too high. Alternatives like GLP-1 agonists or DPP-4 inhibitors offer similar glucose control without increasing infection risk. Always tell your doctor about your infection history before starting any new diabetes drug.
How soon after starting SGLT2 inhibitors do infections usually appear?
Most genital yeast infections show up within the first 1 to 3 months. UTIs can happen anytime, but the highest risk is in the first 6 months. The FDA found that the median time to a serious infection like urosepsis was 45 days after starting the drug. That’s why it’s critical to monitor symptoms closely during the first few months and report anything unusual right away.
Can cranberry juice prevent UTIs from SGLT2 inhibitors?
Cranberry supplements-specifically standardized extracts with proanthocyanidins-have been shown in a 2023 FDA safety update to reduce UTI incidence by 29% in people taking SGLT2 inhibitors. However, cranberry juice alone is not enough. Most store-bought juices are too sugary and diluted to help. If you want to try it, use a daily 500 mg cranberry capsule. It’s not a guarantee, but it’s a low-risk addition that many doctors now recommend.
Is it safe to restart an SGLT2 inhibitor after having a serious infection?
It’s generally not recommended. In documented cases, patients who restarted SGLT2 inhibitors after a severe infection like emphysematous pyelonephritis or Fournier’s gangrene had recurrence within months. The drug itself is the trigger. Even if you’re fully healed, the risk of another life-threatening infection is too high. Your doctor should consider switching you to a different class of diabetes medication permanently.
What Comes Next?
The future of diabetes care is getting smarter. Researchers are now testing dual SGLT1/2 inhibitors that reduce glucose absorption earlier in the digestive tract-meaning less sugar ends up in the urine. Early results look promising. There are also new risk-prediction tools being developed that can tell you, before you even start, whether you’re likely to get an infection.
For now, the message is clear: SGLT2 inhibitors are powerful tools-but they’re not for everyone. Know your risks. Listen to your body. And never ignore a symptom just because you’re told the drug is "safe." Your health isn’t a statistic. It’s your life.