TIA Vision Symptom Assessment Tool
Assess Your Vision Symptoms
Results & Action Plan
Enter your symptoms to see urgency assessment
A transient ischemic attack (TIA) often flies under the radar, but it can send a clear warning signal through your eyes. Suddenly losing part of your vision or seeing a curtain fall across your sight isn’t just an eye issue - it can be the brain’s SOS before a full‑blown stroke.
Key Takeaways
- TIAs can cause temporary vision loss, double vision, or visual field defects.
- Common eye symptoms include amaurosis fugax, diplopia, and sudden blind spots.
- Underlying causes often involve carotid artery disease, atherosclerosis, hypertension or diabetes.
- Any abrupt visual change deserves immediate medical attention - treat it as a potential stroke.
- Managing risk factors and regular vascular screening reduce both TIA and vision‑related complications.
What Is a Transient Ischemic Attack?
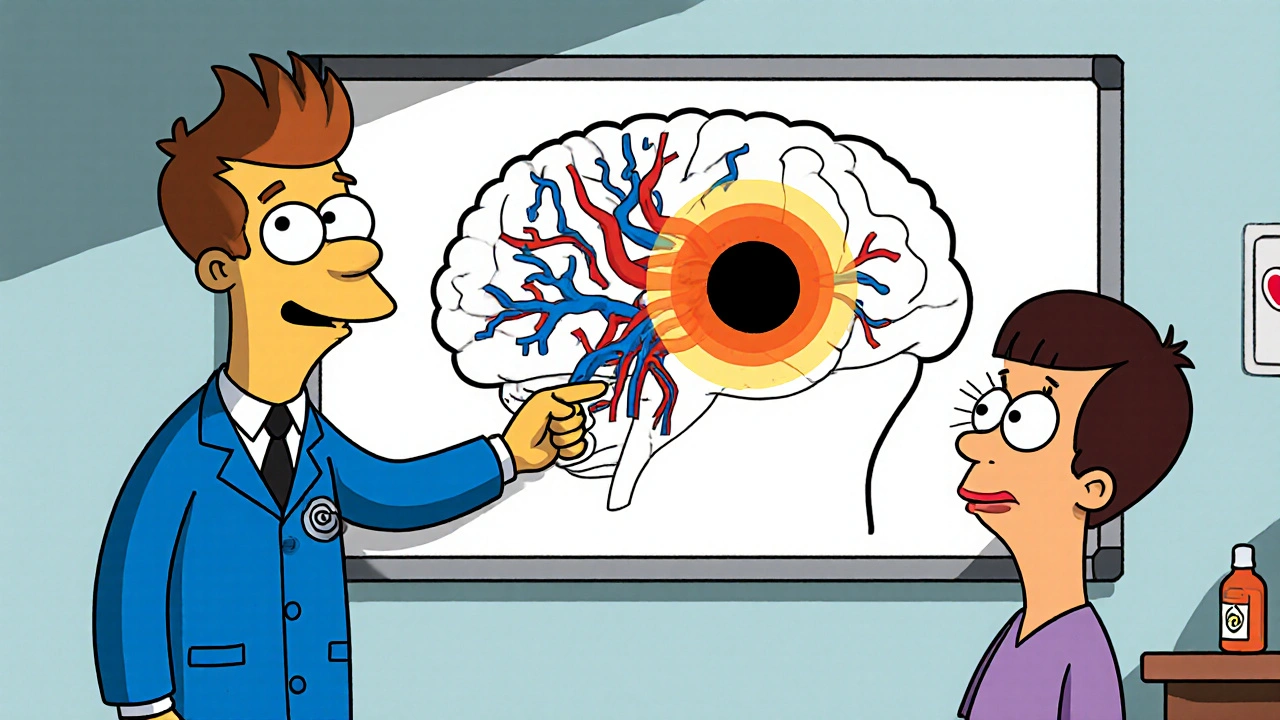
Transient Ischemic Attack is a brief interruption of blood flow to a part of the brain, usually lasting less than 24 hours and leaving no permanent damage. Although symptoms resolve quickly, the event is a strong predictor of a future stroke - up to 40% of patients experience a stroke within the next five years. The most common underlying mechanisms are blood clots, atherosclerotic plaque, or sudden drops in blood pressure that starve brain tissue.
Why the Eyes Get Involved
Vision is controlled by the occipital cortex and the optic pathways, both of which receive blood from the internal carotid and vertebral arteries. When a TIA compromises these vessels, the visual centers can be starved of oxygen for a few minutes, leading to distinct eye symptoms.
Vision Problems in the context of a TIA refer to any sudden, reversible change in visual perception caused by fleeting cerebral ischemia. Because the brain processes visual information in real time, even a short‑lived blockage can produce dramatic, yet temporary, visual loss.
Common Eye Symptoms Linked to TIA
The visual clues can point directly to the vessel involved. Below is a quick rundown of the most frequent presentations:
- Amaurosis Fugax - a curtain‑like gray shade that sweeps over one eye for seconds to minutes. It’s often called a “shimmering veil” and signals emboli from the carotid artery.
- Diplopia (double vision) - usually horizontal and indicating brain‑stem or cranial nerve ischemia.
- Visual Field Defect - sudden loss of half the visual field (hemianopia) on one side, hinting at posterior cerebral artery involvement.
- Transient Blurred Vision - fuzzy sight affecting both eyes, commonly tied to overall blood pressure drops.
Underlying Vascular Conditions
Understanding the root causes helps clinicians decide the urgency and the preventive steps. The most important related entities are:
Retinal Ischemia occurs when the tiny retinal arteries receive insufficient blood, often mirroring a carotid blockage.
Amaurosis Fugax is actually a form of retinal ischemia caused by emboli that briefly lodge in the ophthalmic artery.
Carotid Artery Stenosis is a narrowing of the carotid arteries due to atherosclerotic plaque, the most common source of emboli that generate eye‑focused TIAs.
Atherosclerosis is the buildup of fatty deposits inside arterial walls, creating a breeding ground for clots and plaque rupture.
Hypertension and Diabetes accelerate atherosclerosis and increase the likelihood of micro‑emboli.
Blood Clot formation can happen in the heart (especially in atrial fibrillation) or within atherosclerotic plaques, traveling to the eye or brain.
Comparison of Typical TIA‑Related Vision Issues
| Symptom | Typical Cause | Duration | Urgency |
|---|---|---|---|
| Amaurosis Fugax | Embolus from carotid artery | Seconds‑minutes | High - stroke risk |
| Diplopia | Brain‑stem ischemia or cranial nerve VI palsy | Minutes‑hours | High - possible basilar artery TIA |
| Hemianopia | Posterior cerebral artery | Minutes‑hours | Very high - imminent stroke |
| Transient blurred vision | Systemic hypotension | Minutes | Moderate - evaluate cardiovascular status |
What to Do If You Experience Sudden Vision Changes
- Stop what you’re doing and sit or lie down - safety first.
- Check the time - note when the symptom started and how long it lasted.
- Call emergency services (999 in the UK). Mention that you have sudden vision loss or double vision and suspect a TIA.
- If you have a known history of atrial fibrillation, high blood pressure, or carotid disease, tell the dispatcher.
- Do not drive or operate heavy machinery until a medical professional clears you.
Even if the vision returns, the episode is a red flag. Hospital evaluation typically includes a CT or MRI scan, carotid Doppler ultrasound, and blood work for cholesterol, glucose, and clotting factors.

Prevention and Long‑Term Management
Reducing the chance of another TIA - and the associated eye problems - revolves around controlling the same risk factors that cause ordinary strokes.
- Blood pressure control: Aim for < 130/80mmHg with lifestyle changes and medication if needed.
- Cholesterol management: Statins are proven to shrink plaque and lower embolic risk.
- Diabetes control: Keep HbA1c under 7% to protect vessel walls.
- Smoking cessation: Each cigarette adds to arterial damage.
- Regular exercise: 150minutes of moderate activity weekly improves circulation.
- Carotid screening: If you’re over 55, have a family history of stroke, or have had a TIA, discuss duplex ultrasound with your GP.
- Aspirin or antiplatelet therapy: Often prescribed after a TIA to stop clot formation.
When to Seek Immediate Care
Any of the following warrants a 999 call:
- Sudden, painless loss of vision in one or both eyes.
- Double vision that appears out of the blue.
- Vision loss lasting longer than a few minutes.
- Associated symptoms such as weakness, speech difficulty, facial droop, or severe headache.
Quick action can turn a TIA into a reversible event and prevent a full‑scale stroke.
Next Steps & Troubleshooting
If you’ve already seen a doctor and received a TIA diagnosis, follow these practical steps:
- Schedule a carotid duplex within two weeks.
- Ask for a comprehensive lipid panel and HbA1c test.
- Set up a medication review - ensure you’re on antiplatelet therapy unless contraindicated.
- Keep a symptom diary - note any repeat visual episodes, even if they resolve.
- Share the diary with your neurologist or vascular surgeon at the next visit.
When symptoms recur despite good control, your doctor may consider more aggressive options such as carotid endarterectomy or stenting.
Frequently Asked Questions
Can a TIA cause permanent vision loss?
Most TIA‑related eye symptoms are temporary, but if the underlying blockage persists long enough, it can lead to permanent retinal or cortical damage. Prompt treatment dramatically reduces that risk.
What’s the difference between amaurosis fugax and a regular eye migraine?
Amaurosis fugax is usually a shade that covers the whole visual field of one eye and is caused by an embolus, while an eye migraine (ocular migraine) presents as flashing lights or scintillating scotomas that move across the field and often affect both eyes.
Should I get an eye exam after a TIA?
Yes. An ophthalmic exam can detect retinal ischemia or embolic debris that might not be obvious to a neurologist, and it helps coordinate care with your vascular team.
How fast does a carotid endarterectomy work?
The surgery removes plaque in a single session and restores normal blood flow immediately, cutting the risk of future TIAs and related eye issues.
Can lifestyle changes alone prevent TIA‑related vision problems?
Lifestyle improvements (diet, exercise, quitting smoking) are essential and can significantly lower risk, but many patients still need medication or procedural interventions for optimal protection.