Swallowing feels natural-until it doesn’t. If you’ve ever felt food stick in your chest, or had to drink water to push down a bite, you might be dealing with something more serious than occasional indigestion. These aren’t just quirks. They’re signs of esophageal motility disorders, where the muscles in your esophagus stop working the way they should. The result? Dysphagia-difficulty swallowing-that can turn meals into stressful, even painful, events.
What Exactly Is Going On in Your Esophagus?
Your esophagus isn’t just a tube. It’s a muscular pipeline that uses coordinated waves of contractions, called peristalsis, to push food down to your stomach. Think of it like squeezing a toothpaste tube from the bottom up. In esophageal motility disorders, those waves get messy, weak, or don’t happen at all. The lower esophageal sphincter (LES)-the valve at the bottom-might also stay clenched when it should open. That’s what causes food to back up. These aren’t rare. About 10% of people who complain of dysphagia end up with some kind of motility issue, even if it’s mild. The most well-known is achalasia, which affects roughly 1 in 100,000 people each year. But there are others: diffuse esophageal spasm, nutcracker esophagus, jackhammer esophagus, and more. Some are rare. Others are common enough that doctors see them regularly.Dysphagia: More Than Just Trouble Swallowing
Dysphagia sounds simple, but it’s not. It’s not just choking or coughing. For people with motility disorders, it often starts with solids-bread, meat, rice-and slowly gets worse until even liquids are hard to swallow. Many report food getting stuck, sometimes for minutes. Regurgitation is common too: undigested food coming back up, often hours after eating. Weight loss follows. Some lose 15 to 20 pounds without trying. Chest pain is another red flag. It doesn’t always feel like heartburn. In disorders like diffuse esophageal spasm, the pain can be sharp, squeezing, and mimic a heart attack. That’s why so many end up in emergency rooms before anyone thinks to check their esophagus. One patient from Boston Medical Center said she visited the ER six times for chest pain before manometry revealed she had jackhammer esophagus. She’d been on proton pump inhibitors (PPIs) for eight years-meds for acid reflux-that did nothing.Why Manometry Is the Gold Standard
If you have dysphagia, your doctor will likely start with an endoscopy. That’s to rule out tumors, strictures, or inflammation. But if everything looks normal, the next step is high-resolution manometry (HRM). This isn’t a simple test. A thin, flexible tube with 36 pressure sensors is passed through your nose into your esophagus. You’ll be asked to swallow sips of water-sometimes 10 or more times. Each sensor records pressure at 1-centimeter intervals, creating a detailed map of how your esophagus moves. It’s like getting a video of your esophagus contracting, but instead of images, you get numbers. The Chicago Classification system, updated in 2023, uses these numbers to diagnose specific disorders. Before HRM, doctors relied on older methods like barium swallows. But those missed up to 22% of achalasia cases. HRM catches 96%. One key part of the test is the Multiple Rapid Swallows (MRS) test. You’ll swallow five quick sips in a row. A healthy esophagus responds by suppressing contractions and relaxing the LES. In disorders like achalasia, that response is absent. That’s a clear signal.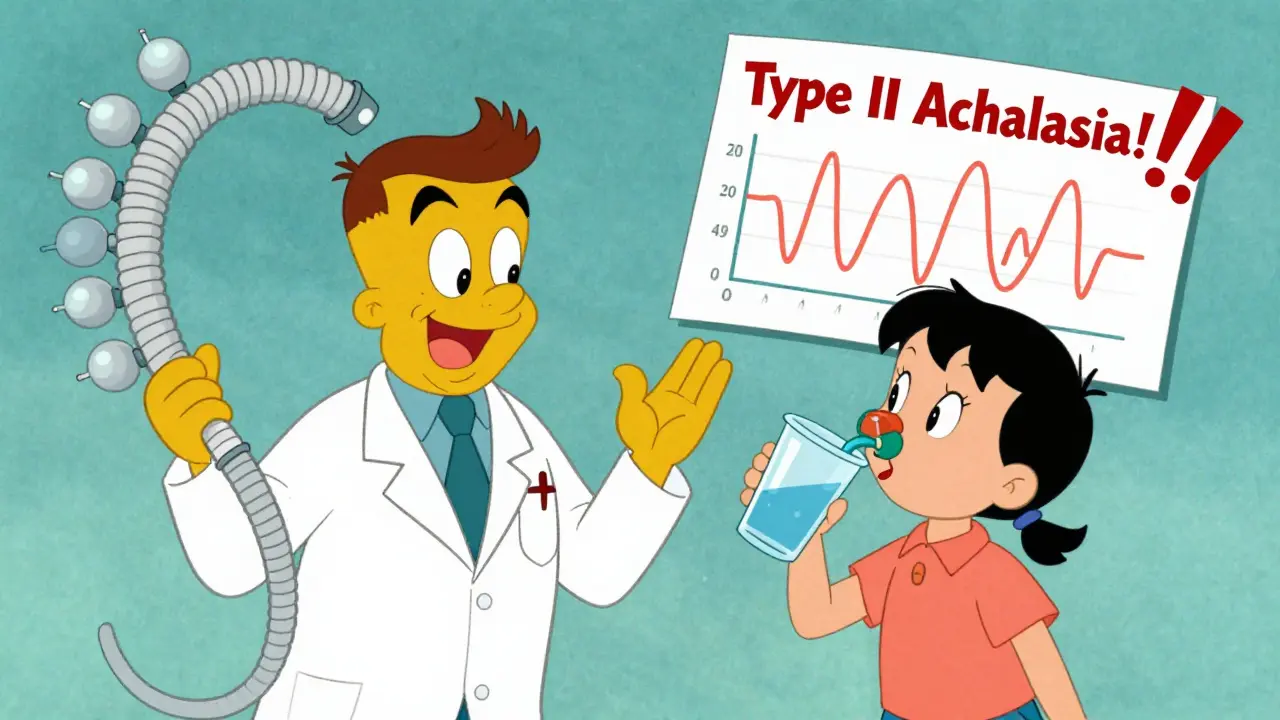
The Chicago Classification v4.0: A New Language for Diagnosis
Before 2008, every doctor interpreted manometry differently. Two experts could look at the same tracing and give different diagnoses. That changed with the Chicago Classification. Developed by a global team led by Dr. John E. Pandolfino, it turned manometry from an art into a science. The 2023 update (v4.0) made things even clearer. It introduced major vs. minor motility disorders. Major ones-like achalasia, jackhammer esophagus, or esophagogastric junction outflow obstruction (EGJOO)-need treatment. Minor ones might just be normal variations. This prevents overdiagnosis. One expert put it bluntly: “We’ve been labeling too many people with ‘abnormal’ motility that doesn’t cause symptoms.” Achalasia is now split into three types:- Type I (classic): No contractions. The esophagus is silent. Seen in 20% of cases.
- Type II: Pan-esophageal pressurization. The whole tube squeezes at once. The most common-70% of cases.
- Type III: Spastic contractions. Chaotic, forceful waves. 10% of cases.
What About Other Tests? EndoFLIP, SmartPill, and More
HRM isn’t the only tool. EndoFLIP (endoluminal functional lumen imaging probe) measures how stretchy your esophagus is. It’s especially helpful when the LES is tight but not fully closed-like in EGJOO. It gives a number called distensibility index. If it’s too low, you likely need intervention. Then there’s the SmartPill-a tiny capsule you swallow. It records pressure and pH as it travels through your gut over 24 to 48 hours. No tube. No discomfort. It’s not as detailed as HRM, but it’s great for people who can’t tolerate the catheter. Studies show it matches HRM in 85% of cases for detecting major disorders. These tools are growing. The global market for esophageal diagnostics is expected to hit $410 million by 2028. But access isn’t equal. In the U.S. and Europe, most academic hospitals have HRM. In rural clinics or low-income countries, it’s still rare. That means many patients wait years for a diagnosis.Treatment: From Surgery to Injections
Treatment depends on the disorder. For achalasia, there are three main options:- Laparoscopic Heller myotomy (LHM): A surgeon cuts the LES muscle through small belly incisions. Success rate: 85-90% at five years. But it can cause reflux.
- Peroral endoscopic myotomy (POEM): A scope goes in through the mouth, cuts the muscle from inside. Just as effective as LHM, but 44% of patients develop reflux within two years.
- Pneumatic dilation: A balloon is inflated in the LES to stretch it. Works in 70-80% of cases, but 30% need repeat procedures within five years.

Why So Many Get Misdiagnosed
The biggest problem? Doctors mistake motility disorders for acid reflux. PPIs are prescribed for years-sometimes decades-before anyone checks the esophagus properly. A survey from the International Foundation for Gastrointestinal Disorders found that 68% of patients waited 2-5 years for a correct diagnosis. 42% saw three or more doctors. One Reddit user wrote: “After my POEM, I ate a burger for the first time in seven years. I cried.” Another on a health forum said: “I was told I had GERD for eight years. Turns out I had jackhammer esophagus. No acid. Just broken muscles.” The fix? Better education. When patients are told what to expect before manometry, satisfaction jumps from 45% to 78%. Doctors need to ask: “Does your swallowing feel weak? Does food get stuck? Does it hurt?” Not just, “Do you have heartburn?”What’s Next?
AI is stepping in. Early tools can analyze manometry tracings and spot achalasia with 92% accuracy-better than untrained doctors. In the next five years, we’ll likely see more home-based testing, better drugs targeting esophageal nerves, and wider access to HRM in community hospitals. But the real breakthrough isn’t technology. It’s awareness. If you’ve had trouble swallowing for months, and PPIs didn’t help, ask for manometry. It’s not a last resort. It’s the first real step toward fixing what’s broken.Can esophageal motility disorders be cured?
Some can be effectively managed, but not always cured. Achalasia, for example, can be treated successfully with surgery or dilation, and most patients regain normal swallowing. But the underlying nerve damage doesn’t reverse. Symptoms stay controlled for years, but relapses can happen. Disorders like jackhammer esophagus often respond to medication or Botox, but long-term relief varies. The goal isn’t always a cure-it’s restoring quality of life.
Is high-resolution manometry painful?
It’s uncomfortable, not usually painful. The tube goes through your nose, which can trigger gagging or a runny nose. Most patients report mild sore throat afterward. About 35% say they felt significant discomfort during the test. Sedation isn’t typically used because you need to be awake to swallow. But if you’re anxious, talk to your doctor-you can get a numbing spray or take a mild relaxant beforehand.
Can I have these disorders without having GERD?
Absolutely. In fact, many people with achalasia or jackhammer esophagus have no acid reflux at all. The problem is muscle function, not stomach acid. That’s why PPIs don’t help. If you’ve been on reflux meds for years with no improvement, motility disorders should be considered. Up to 40% of patients with dysphagia and normal endoscopy turn out to have motility issues-not GERD.
How long does it take to get results from manometry?
The test itself takes about 30 minutes. But interpretation is complex. A trained specialist needs to review the pressure maps, check for patterns, and apply the Chicago Classification criteria. Most clinics take 3-7 days to return results. In busy centers, it can take up to two weeks. Don’t assume the test is normal just because you felt fine afterward. The data tells the real story.
Are there non-invasive alternatives to manometry?
There are some, but none are as accurate. The SmartPill capsule is the best non-invasive option-it measures pressure and pH as it moves through your gut. It’s good for screening, especially if you can’t tolerate the tube. But it doesn’t show the fine details of peristalsis like HRM does. Barium swallows are still used sometimes, but they miss subtle contractions. For a definitive diagnosis, HRM remains the gold standard.
Can stress or anxiety cause esophageal motility disorders?
Stress doesn’t cause these disorders, but it can make symptoms worse. If you have achalasia or nutcracker esophagus, anxiety can increase chest pain or make swallowing feel harder. That’s because the nerves controlling your esophagus are sensitive to stress signals. But the root cause is physical-nerve damage, muscle fibrosis, or genetic factors-not psychological. Treating anxiety helps with comfort, but not the underlying issue.
What happens if I ignore my symptoms?
Ignoring dysphagia can lead to serious complications. Food backing up can cause aspiration pneumonia if it enters your lungs. Chronic pressure in the esophagus can lead to dilation or even a rare cancer called esophageal squamous cell carcinoma, especially in long-standing achalasia. Weight loss and malnutrition are common. The longer you wait, the more your esophagus stretches and weakens-making treatment harder. Early diagnosis means better outcomes.