On January 1, 1995, a global rule changed how medicines are made, sold, and who can afford them. The TRIPS Agreement - part of the World Trade Organization’s founding treaties - forced every member country to grant 20-year patents on pharmaceuticals. Before that, countries like India, Brazil, and Thailand could make cheap copies of life-saving drugs. After TRIPS, those copies vanished overnight. The result? Millions couldn’t afford HIV meds, cancer treatments, or insulin - not because the science wasn’t there, but because the law said no.
What TRIPS Actually Does
The TRIPS Agreement doesn’t just cover medicines. It sets global rules for patents, trademarks, and copyrights. But when it comes to drugs, its impact is brutal. Article 33 requires all WTO members to give drug patents for at least 20 years from the filing date. That means even if a medicine was invented in the U.S. in 2005, no other country can legally make a cheaper version until 2025 - even if the disease is killing people in real time. Article 27 says patents can’t be denied just because a drug is a "discovery" of a natural substance. That sounds fair - until you realize it lets companies patent tiny chemical tweaks to old drugs. A company might take a 40-year-old painkiller, change one atom, and call it "new." Then they get another 20 years of monopoly pricing. This isn’t innovation. It’s legal maneuvering. And here’s the catch: TRIPS doesn’t care if a country can’t afford the drug. It doesn’t care if a child dies because the price is $1,000 a dose. It only cares about protecting corporate rights.The Flexibilities That Don’t Work
In 2001, after global outrage over AIDS deaths in Africa, WTO members agreed to the Doha Declaration. It said public health emergencies override patent rights. That was the promise. But the real power? It was in the fine print. Article 31 lets countries issue compulsory licenses - basically, a government can say, "We’re making this drug anyway, even without the patent holder’s permission." But there’s a twist: Article 31f says the medicine can only be made for the domestic market. So if you’re a small African country with no drug factories, you’re out of luck. You can’t import generics from India, even if they’re cheaper and proven safe. That’s why the 2005 amendment was created - Article 31bis. It was supposed to fix this. Now, countries without manufacturing capacity could import generics made under compulsory license. Sounds perfect, right? It’s not. Only one country has ever used it: Rwanda, in 2008. They needed HIV meds. Canada agreed to make them. But the paperwork? It took four years. Twelve government agencies. Dozens of forms. Legal reviews. Political pressure. The final cost? Still 30% higher than if Rwanda had its own factory. Médecins Sans Frontières called it "unworkable." And they’re not alone. A 2019 Duke University study found that 92% of low-income countries have no one full-time staffed to handle these applications. No one knows how to file. No one has the time. No one wants to risk being punished by the U.S. or EU.What Happens When Countries Try
Thailand tried in 2006. They issued compulsory licenses for three drugs: efavirenz (HIV), clopidogrel (heart), and imatinib (cancer). Prices dropped by 30% to 80%. Then the U.S. slapped them with trade sanctions. They lost $57 million a year in export benefits. Thailand backed down. Brazil did the same in 2007 with efavirenz. Got a 60% price cut. The U.S. put Brazil on its "Priority Watch List" for two years. No one got arrested. No laws were broken. But the message was clear: Don’t challenge the system. South Africa almost did it in 1997. They passed a law allowing parallel imports and compulsory licensing. Thirty-nine pharmaceutical companies sued them. The case made headlines worldwide. Public pressure mounted. The companies dropped the lawsuit. But the threat worked. Many other countries never even tried. The pattern? Try to save lives. Get punished economically. Stay silent. Keep paying.
Voluntary Licensing: A Band-Aid on a Broken System
Pharmaceutical companies now offer "voluntary licenses" through the Medicines Patent Pool (MPP). It sounds like a win-win. Companies let generic makers produce their drugs in poor countries. MPP negotiates the deals. But here’s the truth: As of 2022, MPP covers only 44 patented medicines - out of thousands. And 73% of those licenses are only valid in sub-Saharan Africa, even though diseases like hepatitis C or diabetes affect people everywhere. Worse, MPP only works for drugs companies are willing to license. They pick the ones that are old, low-margin, or already losing patent protection. The new, expensive cancer drugs? Not on the list. The next-generation HIV pills? Still locked up. Voluntary licensing isn’t access. It’s charity. And charity can be taken away at any time.TRIPS-Plus: The Hidden Rules
Here’s the real kicker: TRIPS is just the baseline. Most rich countries now push "TRIPS-plus" terms into bilateral trade deals. The U.S.-Jordan Free Trade Agreement, signed in 2011, forced Jordan to extend patent terms beyond 20 years. It blocked generic approval until the patent expired - even if the drug was never sold there. Similar clauses are now in deals with Colombia, Morocco, Peru, and 141 other countries. On average, these deals add 4.7 extra years of monopoly control. That’s not innovation. That’s rent-seeking. A 2019 study estimated these extra protections cost low- and middle-income countries $2.3 billion a year in lost savings from generics. That’s enough to treat 11 million people with HIV for a year.The Human Cost
Two billion people still can’t get the medicines they need. Eighty percent of that gap? Directly tied to patent rules. In 2022, the global pharmaceutical market hit $1.42 trillion. Patented drugs made up 68% of that revenue - even though they account for only 12% of prescriptions. Meanwhile, in low-income countries, generics make up just 28% of prescriptions. In the U.S.? 89%. Why? Because in the U.S., you can buy a generic version of Lipitor for $10. In Malawi, the same drug costs $1,000 - if you can find it at all. The numbers don’t lie. The system works perfectly - for companies. It fails completely for people.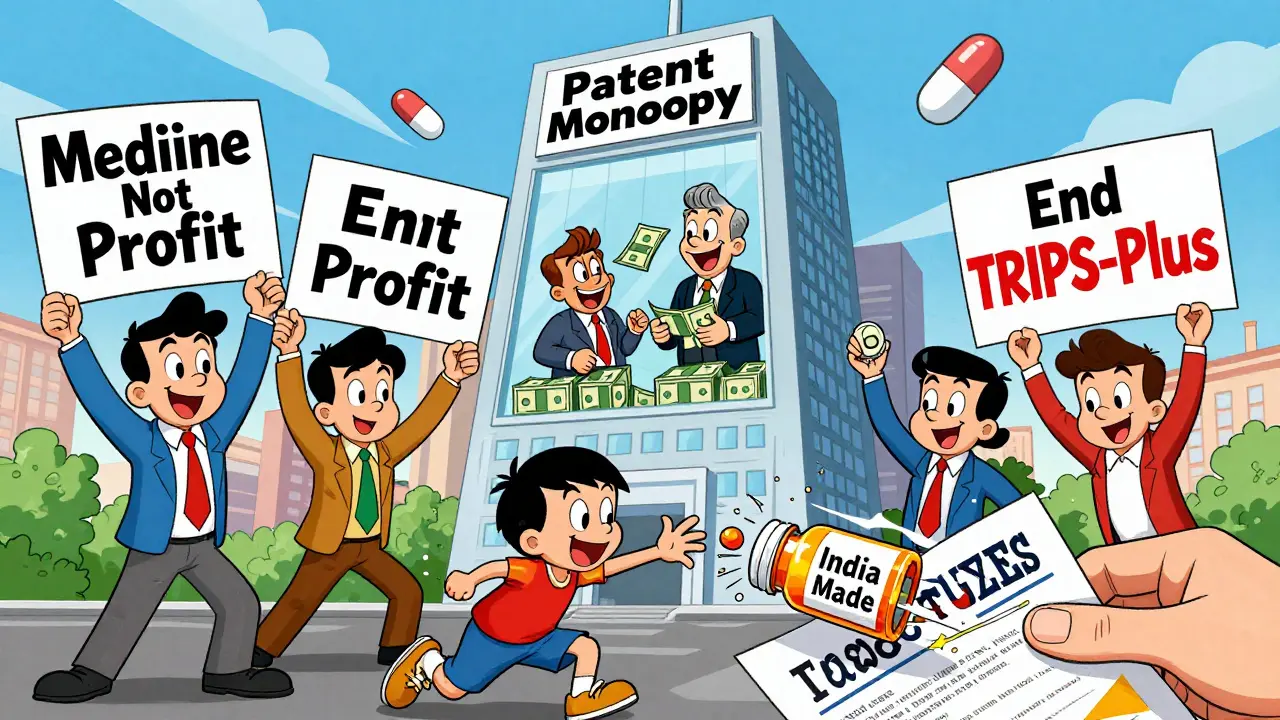
Is There Any Hope?
In 2020, India and South Africa asked the WTO to waive TRIPS rules for COVID-19 vaccines and treatments. After two years of delays, the WTO agreed - but only for vaccines. Not diagnostics. Not therapeutics. Not future pandemics. That’s a start. But it’s not enough. The UN’s 2024 Pandemic Meeting called for TRIPS reform. The WHO’s 2023 Digital Health Strategy now says flexibilities should apply to digital health tech too. That’s a sign the debate is expanding. The old model - patents as absolute rights - is crumbling. But change won’t come from goodwill. It will come from pressure. From protests. From governments refusing to back down. From countries building their own generic factories. From civil society demanding transparency. The TRIPS Agreement was never about health. It was about control. And control is what’s being challenged now.What Needs to Change
Here’s what real reform looks like:- Remove Article 31f - let countries import generics freely.
- Abolish TRIPS-plus clauses in all trade deals.
- Require patent holders to disclose all clinical trial data publicly - no more hiding failures.
- Make compulsory licensing automatic during public health emergencies - no paperwork, no delays.
- Extend the LDC transition period permanently - no more deadlines for the poorest.
Can a country legally make generic drugs under TRIPS?
Yes. TRIPS allows compulsory licensing under Article 31, which lets governments authorize generic production without the patent holder’s consent. But there are strict conditions: the license must be for domestic use only (unless using the 2005 amendment), adequate payment must be made to the patent owner, and the process requires complex government notifications. In practice, political pressure and legal complexity make this extremely difficult for most countries.
Why hasn’t the Article 31bis system worked?
It’s been used only once - Rwanda importing HIV drugs from Canada in 2008. The process took four years, involved 78 bureaucratic steps, and required international NGOs to guide the paperwork. Most countries lack staff, legal expertise, or political courage to go through it. The system was designed to be hard, and it succeeded. It’s not broken by accident - it’s broken by design.
Do pharmaceutical companies lose money when generics are made?
They lose potential future profits, but not actual research costs. Most drugs are developed with public funding - NIH in the U.S. spent over $100 billion on biomedical research between 2000 and 2020. Companies then patent the results and charge 100x the production cost. Generic manufacturers pay nothing for R&D. They just replicate the formula. The high price isn’t about recouping costs - it’s about maximizing profit.
Why do rich countries oppose TRIPS flexibilities?
Because their pharmaceutical industries are major exporters. The U.S., Germany, and Switzerland earn billions from patented drug sales. If generics become common, those profits vanish. Trade pressure, sanctions, and diplomatic threats are tools to keep the system intact. The argument that patents drive innovation is used to justify this - but data shows most breakthroughs come from public labs, not private R&D.
Are there any countries successfully producing generics despite TRIPS?
Yes. India is the world’s largest supplier of generic drugs, producing 20% of all generics globally. Brazil, Thailand, and South Africa have all produced generics domestically under compulsory licenses - despite pressure. China and Turkey are expanding their capacity. But these are exceptions. Most countries still rely on imports and pay inflated prices because they lack the legal or political strength to challenge the system.




