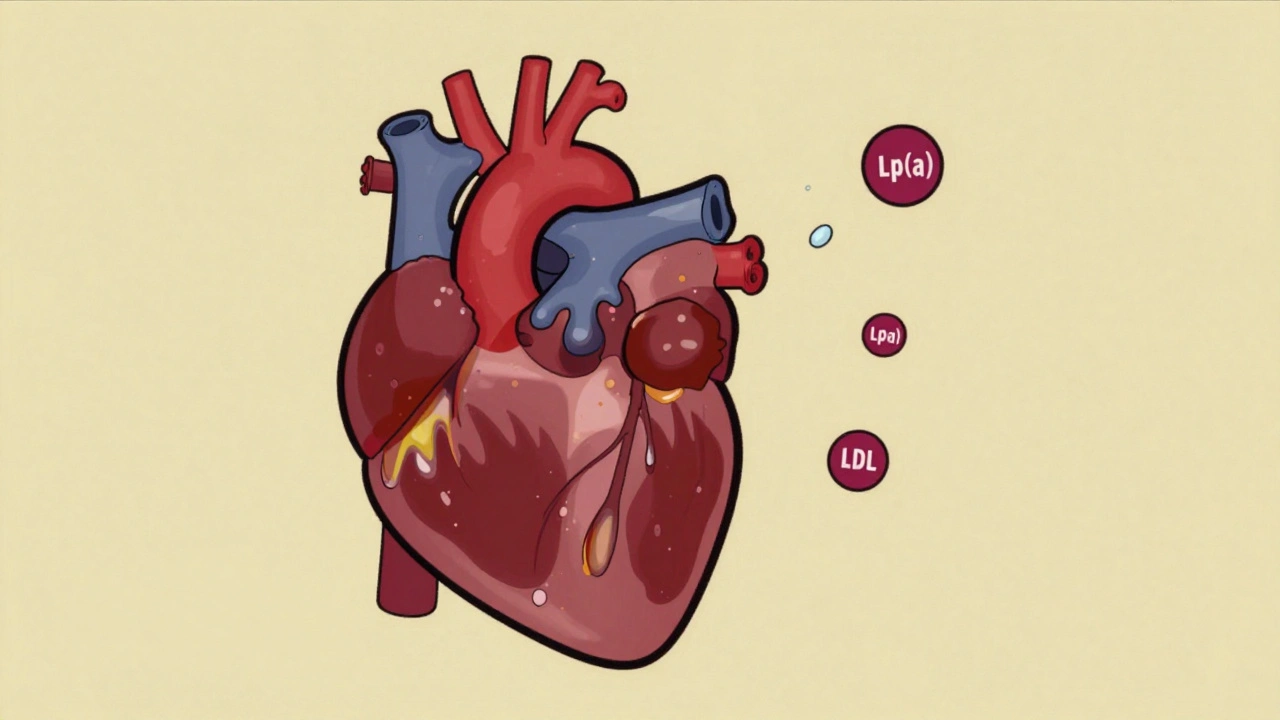
Most people know about LDL cholesterol - the so-called "bad" cholesterol - and how it contributes to heart disease. But there’s another cholesterol-related particle hiding in plain sight, one that’s just as dangerous and completely out of your control: lipoprotein(a), or Lp(a). Unlike LDL, which you can lower with diet, exercise, or statins, Lp(a) is mostly written into your DNA. And if you have high levels, you’re at significantly higher risk for a heart attack or stroke - even if everything else about your cholesterol looks fine.
What Exactly Is Lipoprotein(a)?
Lipoprotein(a), or Lp(a), is a type of lipoprotein that carries cholesterol and fats through your blood. It looks a lot like LDL cholesterol, but it has an extra protein attached - apolipoprotein(a). This extra piece makes Lp(a) sticky and dangerous. It doesn’t just clog arteries like LDL; it also promotes inflammation, helps clots form, and interferes with your body’s ability to break them down.
Think of it this way: LDL is like dirt building up on a road. Lp(a) is like dirt plus glue - it sticks harder, builds faster, and makes it harder to clean up. That’s why even people with otherwise healthy cholesterol levels can have heart attacks if their Lp(a) is high.
It was first discovered in 1963 by Swedish researcher Kare Berg, but for decades, doctors barely paid attention. Today, we know better. Around 20% of people worldwide have elevated Lp(a) levels - that’s one in five. And it’s not rare in any one group; it’s just under-tested.
Why You Might Have High Lp(a) - And Why You Can’t Fix It With Diet
Your Lp(a) level is determined mostly by your genes - 70% to 90% of it, according to research from UC Davis Health. That means if your mom or dad had high Lp(a), you likely inherited it too. It’s passed down in an autosomal dominant pattern, so if one parent has it, you have a 50% chance of getting it.
And here’s the hard truth: you can’t lower Lp(a) with a better diet, more walking, or losing weight. Statins - the most common cholesterol drugs - barely touch it. In fact, some people see their Lp(a) levels go up slightly when they take statins. Niacin can lower it by 20-30%, but it causes flushing, liver issues, and doesn’t clearly reduce heart attacks in trials.
That’s why Lp(a) flies under the radar. Doctors don’t test for it unless you ask. Standard cholesterol panels don’t include it. You need a specific blood test - and most people never get one.
How High Is Too High?
There’s no single "normal" level for Lp(a), but experts agree on clear danger zones:
- 50 mg/dL (105 nmol/L) or higher = increased risk of heart attack or stroke
- 90 mg/dL (190 nmol/L) or higher = very high risk - similar to someone with familial hypercholesterolemia
- 130-391 mg/dL (280-849 nmol/L) = risk equivalent to having inherited high cholesterol from birth
These numbers aren’t guesses. They’re backed by large studies showing that for every 50 mg/dL increase in Lp(a), your risk of heart disease goes up by about 20-30%. And the higher you go, the worse it gets.
There’s also a simple formula to convert between measurement units: Lp(a) in nmol/L = 2.18 × Lp(a) in mg/dL - 3.83. If your lab report gives you one unit and your doctor talks in another, this helps you compare.

Who Should Be Tested?
Because Lp(a) is genetic and silent, screening is critical for people with warning signs:
- Family history of early heart disease (before age 55 in men, 65 in women)
- Personal history of heart attack, stroke, or peripheral artery disease without clear causes
- Diagnosis of familial hypercholesterolemia
- Calcified aortic valve (aortic stenosis), especially if diagnosed young
- Recurrent cardiovascular events despite normal LDL levels
Some experts, including Dr. Gregory Schwartz from the University of Colorado, now recommend that all adults get tested once in their lifetime. That’s because if you don’t know your Lp(a), you can’t manage your risk - and you might pass on a silent danger to your kids.
Demographics and Lp(a): Who’s at Higher Risk?
Lp(a) doesn’t affect everyone equally. Black populations have, on average, much higher levels than white, Hispanic, or Asian populations. Women tend to see their Lp(a) rise after menopause - likely because estrogen helps suppress it. So a woman in her 50s with no other risk factors might suddenly have elevated Lp(a) simply because her hormones shifted.
That doesn’t mean one group is "worse" than another. It means the risk threshold is the same for everyone: higher level = higher risk. A Black woman with Lp(a) of 120 mg/dL has the same elevated risk as a white man with the same level. The numbers don’t care about race or gender - only the level.
What Happens When Lp(a) Is High?
High Lp(a) doesn’t just raise your chance of a heart attack. It’s linked to several serious conditions:
- Coronary artery disease - plaques form faster and are more unstable
- Stroke - clots form more easily and stick harder
- Peripheral artery disease - reduced blood flow to legs and arms
- Aortic valve stenosis - Lp(a) contributes to calcium buildup on the heart’s main valve, making it stiff and narrow
One study found that people with Lp(a) over 125 nmol/L were twice as likely to develop aortic stenosis over 10 years compared to those with normal levels. That’s not a small risk - it’s a major driver of valve disease.

Current Treatment Options - and What’s Coming
Right now, the best treatment for high Lp(a) is managing everything else you can control:
- Keep LDL cholesterol as low as possible (often with high-dose statins or PCSK9 inhibitors)
- Don’t smoke
- Control blood pressure
- Manage diabetes if you have it
- Maintain a healthy weight
These won’t lower Lp(a), but they reduce the overall burden on your arteries. Think of it like wearing a seatbelt - it doesn’t stop the crash, but it saves your life when it happens.
There’s new hope on the horizon. A new class of drugs called antisense oligonucleotides (ASOs) is showing dramatic results. One drug, pelacarsen, reduced Lp(a) by up to 80% in early trials. The big phase 3 trial - called the Lp(a) HORIZON Outcomes Trial - is now underway. It’s testing whether lowering Lp(a) with pelacarsen actually prevents heart attacks and strokes in high-risk patients. Results are expected in 2025.
If the trial succeeds, this could be the first treatment ever approved specifically to target Lp(a). That’s a game-changer.
What You Can Do Today
Even without a specific drug, you’re not powerless. Here’s what to do right now:
- Ask your doctor for an Lp(a) test - especially if you have any of the risk factors above. Don’t wait for them to bring it up.
- Get your LDL down - if your Lp(a) is high, your LDL needs to be as low as possible to compensate.
- Know your family history - talk to relatives about heart disease, strokes, or early deaths. If it’s common, get tested.
- Stay active and eat well - not to lower Lp(a), but to reduce your total cardiovascular risk.
- Track your numbers - keep a record of your Lp(a), LDL, blood pressure, and other markers. Share them with your doctor.
And if you’re a parent with high Lp(a)? Talk to your kids. Tell them about this. Have them tested when they turn 20. Early knowledge saves lives.
Why This Matters More Than Ever
Heart disease is still the leading cause of death worldwide. But many people who die from it had "normal" cholesterol tests. Lp(a) explains why.
For years, we’ve blamed poor diet, lack of exercise, or bad luck. But for one in five people, the real culprit is a genetic gift they never asked for. The good news? We’re finally catching up. Science is no longer ignoring Lp(a). We’re learning how to measure it, understand it, and - soon - treat it.
If you’ve had a heart event with no clear cause, or if your family has a history of early heart disease, this isn’t just another cholesterol number. It’s a signal. And ignoring it could cost you your life - or your children’s.
The clock is ticking. The test is simple. The stakes are high. Don’t wait for a crisis to ask the question: "What’s my Lp(a)?"
Is lipoprotein(a) the same as LDL cholesterol?
No. While Lp(a) contains an LDL-like particle, it has an extra protein called apolipoprotein(a) attached to it. This makes Lp(a) more likely to cause plaque buildup, trigger inflammation, and promote blood clots. Unlike LDL, Lp(a) levels are mostly determined by genetics and aren’t affected by diet or statins the same way.
Can I lower my Lp(a) with diet or exercise?
No. Unlike LDL or triglycerides, Lp(a) levels are not meaningfully changed by lifestyle changes like diet, exercise, or weight loss. Some studies suggest minor fluctuations due to hormones or liver disease, but these are inconsistent. The main focus should be lowering other risk factors - especially LDL cholesterol - to reduce overall heart disease risk.
Who should get tested for Lp(a)?
Anyone with a family history of early heart disease, personal history of heart attack or stroke with normal cholesterol, diagnosed familial hypercholesterolemia, or aortic valve stenosis should be tested. Many experts now recommend a one-time test for all adults, since Lp(a) is so common and strongly genetic.
Are Lp(a) tests covered by insurance?
Coverage varies. In the UK and US, many insurers will cover the test if you have a personal or family history of early cardiovascular disease. However, because it’s not part of routine panels, you may need to request it specifically. Ask your doctor to order it as "Lp(a) quantitative" or "Lp(a) by immunoassay" - not just a standard lipid panel.
Will new drugs for Lp(a) be available soon?
The most promising drug, pelacarsen, is in a large phase 3 clinical trial called Lp(a) HORIZON. Results are expected in 2025. If the trial shows that lowering Lp(a) reduces heart attacks and strokes, this drug could be approved by 2026. Other therapies are also in development, but pelacarsen is the closest to market.
Can Lp(a) be inherited from just one parent?
Yes. Lp(a) is inherited in an autosomal dominant pattern. That means if one parent has a gene variant that causes high Lp(a), each child has a 50% chance of inheriting it. You don’t need to get it from both parents - just one is enough to raise your risk significantly.
Is high Lp(a) more dangerous than high LDL?
It’s not necessarily "more" dangerous - but it’s independent and additive. High LDL causes plaque. High Lp(a) makes that plaque more unstable and increases clotting. Someone with both high LDL and high Lp(a) has a much higher risk than someone with just one. Even with normal LDL, high Lp(a) still raises heart attack risk.
Does Lp(a) affect women differently than men?
Yes. Estrogen suppresses Lp(a), so levels often rise in women after menopause - sometimes by 20-30%. This may partly explain why heart disease risk increases sharply in women after age 50. Men tend to have stable levels throughout life, but they’re still at risk if their levels are high. Gender doesn’t change the risk threshold - just the timing of when levels may spike.