When someone is prescribed opioids for chronic pain, the goal isn’t just to manage pain-it’s to keep them safe. But opioids carry real risks: addiction, overdose, and misuse. That’s why doctors don’t just write a prescription and walk away. They monitor. And one of the most common tools they use? Urine drug screens.
Why Urine Drug Screens Are Routine in Opioid Treatment
Urine drug testing isn’t about suspicion. It’s about clarity. A simple urine sample can tell a doctor whether a patient is taking their prescribed medication as directed-or using something they weren’t supposed to. This isn’t just paperwork. It’s a safety net. The CDC, American Society of Addiction Medicine, and other leading groups all recommend urine testing for patients on long-term opioid therapy. Why? Because data shows that people taking opioids are at higher risk of overdose, especially when other substances like benzodiazepines, alcohol, or synthetic opioids like fentanyl are mixed in. In 2021, over 80,000 overdose deaths in the U.S. involved opioids. Many of those could have been prevented with better monitoring. Urine tests help catch hidden risks. Maybe a patient is taking extra pills because the dose isn’t working. Maybe they’re using street drugs to cope. Or maybe they’re selling their pills. Without testing, these behaviors stay invisible. With testing, doctors can adjust treatment before something goes wrong.How Urine Tests Work: Immunoassays vs. Confirmatory Testing
Not all urine tests are the same. There are two main types: screening tests and confirmatory tests. Screening tests, usually immunoassays like EMIT, are fast and cheap-around $5 per test. They give results in hours. But they’re not perfect. Up to 30% of them give false positives. That means a patient might test positive for opioids even if they never took them. Why? Over-the-counter meds like ibuprofen, poppy seeds, or even some antibiotics can trigger misleading results. The bigger problem? False negatives. Many standard screens can’t detect hydrocodone, oxycodone, or fentanyl properly. One study found that 72% of patients who were taking hydrocodone tested negative on routine screens. That’s not a mistake-it’s a flaw in the test. Patients get accused of non-compliance when they’re actually doing exactly what they were told. That’s where confirmatory testing comes in. Gas Chromatography/Mass Spectrometry (GC/MS) and Liquid Chromatography/Mass Spectrometry (LC-MS) are the gold standards. These tests cost more-$25 to $100 per sample-but they can identify exact drugs and metabolites. They’re the only way to confirm whether fentanyl is truly present, or whether a patient’s oxycodone levels match their prescription. Doctors often use both: a cheap screen first, then a confirmatory test if something looks off. But too many clinics skip the confirmation. That’s where patients get wrongly labeled as non-adherent-and sometimes even cut off from care.Fentanyl: The Silent Gap in Standard Tests
Fentanyl is the biggest challenge in opioid monitoring today. It’s 50 to 100 times stronger than morphine. It’s in counterfeit pills. It’s in street drugs. And until recently, most urine screens couldn’t detect it at all. Standard opiate panels were designed for morphine and codeine. Fentanyl’s chemical structure is completely different. So even if a patient is using a fentanyl patch or taking illicit fentanyl, their test might come back clean. This isn’t a glitch-it’s a systemic blind spot. In 2023, the FDA approved the first fentanyl-specific immunoassay. It’s 98.7% accurate at detecting fentanyl at very low levels. But many clinics haven’t upgraded yet. A doctor in Birmingham told me last month that half his fentanyl patch patients still test negative on routine panels. He now orders LC-MS for every one of them-adding $80 to each test, and pushing back on insurance denials. Until every clinic switches to fentanyl-aware panels, patients on synthetic opioids are at risk of being misunderstood-and possibly punished-for something they didn’t even know was undetectable.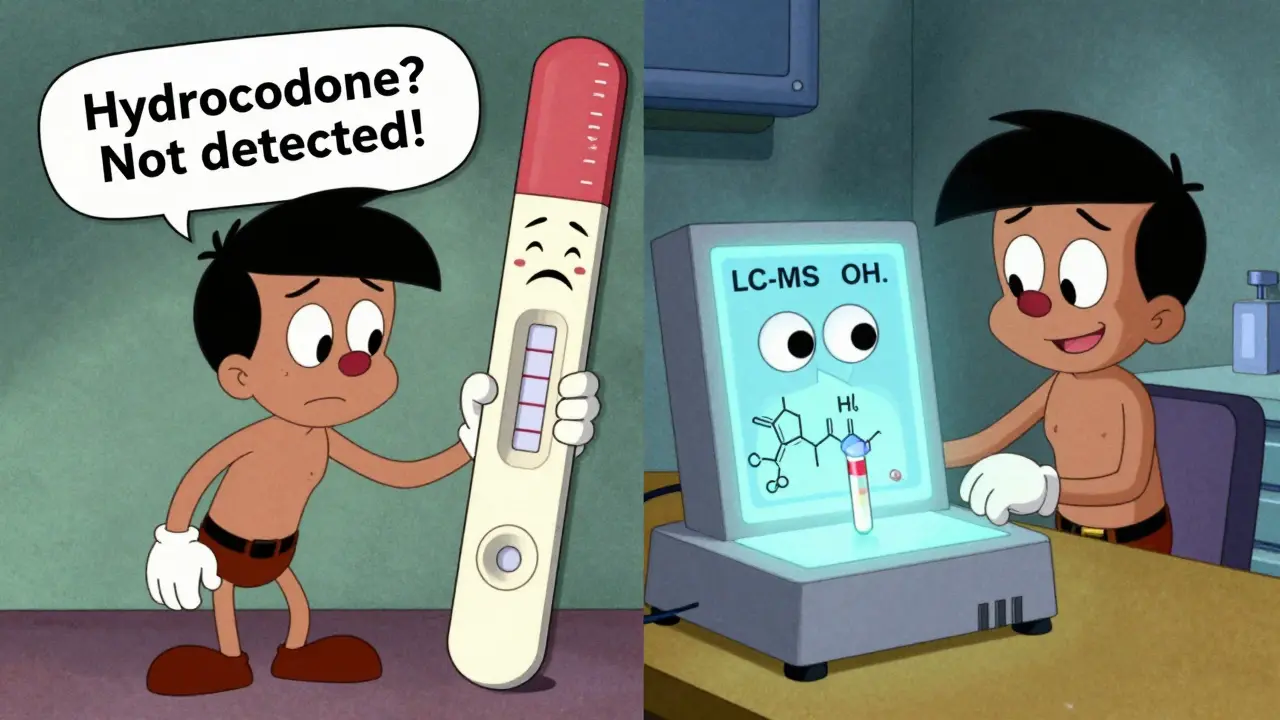
Risk Stratification: Who Gets Tested and How Often?
Not every patient needs the same level of monitoring. That’s where risk stratification comes in. The Opioid Risk Tool (ORT) is a simple five-question survey used in clinics across the U.S. and U.K. It asks about personal or family history of substance use, age, mental health conditions, and past trauma. Based on the answers, patients are grouped into low, moderate, or high risk. - Low-risk patients: annual urine testWhat the Test Doesn’t Tell You
Urine tests can’t tell you if someone is in pain. They can’t tell you if their dose is too high or too low. They can’t tell you if the medication is working. That’s why some doctors make the mistake of treating a negative test as proof of non-adherence. But here’s the truth: a negative result doesn’t always mean the patient skipped their meds. It could mean the test didn’t detect it. Or they took it too long ago. Or their body metabolizes it differently. Quantitative testing-measuring exact drug levels-isn’t useful for judging adherence. A patient taking 20 mg of oxycodone daily might have low levels in their urine because they metabolize it quickly. Another patient taking the same dose might have high levels because they metabolize it slowly. Neither is right or wrong. Just different. The goal isn’t to catch people breaking rules. It’s to understand their story.Real Problems Clinicians Face
Behind the data are real people and real frustrations. One patient on Reddit, ‘ChronicPainWarrior22’, wrote: “I took my oxycodone like clockwork. My test came back negative. They accused me of lying. I lost my prescription for three months.” He later found out his lab used an outdated immunoassay that couldn’t detect oxycodone metabolites properly. Another doctor on a medical forum said: “I had a patient on buprenorphine. Her test showed amphetamines. She didn’t use them. Turns out, buprenorphine can cross-react with amphetamine screens. We didn’t know until we ran a confirmatory test.” These aren’t rare cases. A 2021 study found 23% of patients on buprenorphine were wrongly disciplined because of false positives. That’s one in four. Clinics that use urine testing well report big wins: fewer lost prescriptions, fewer ER visits, fewer overdoses. One practice in Birmingham saw a 37% drop in lost opioid prescriptions after switching to risk-based testing with confirmatory follow-ups.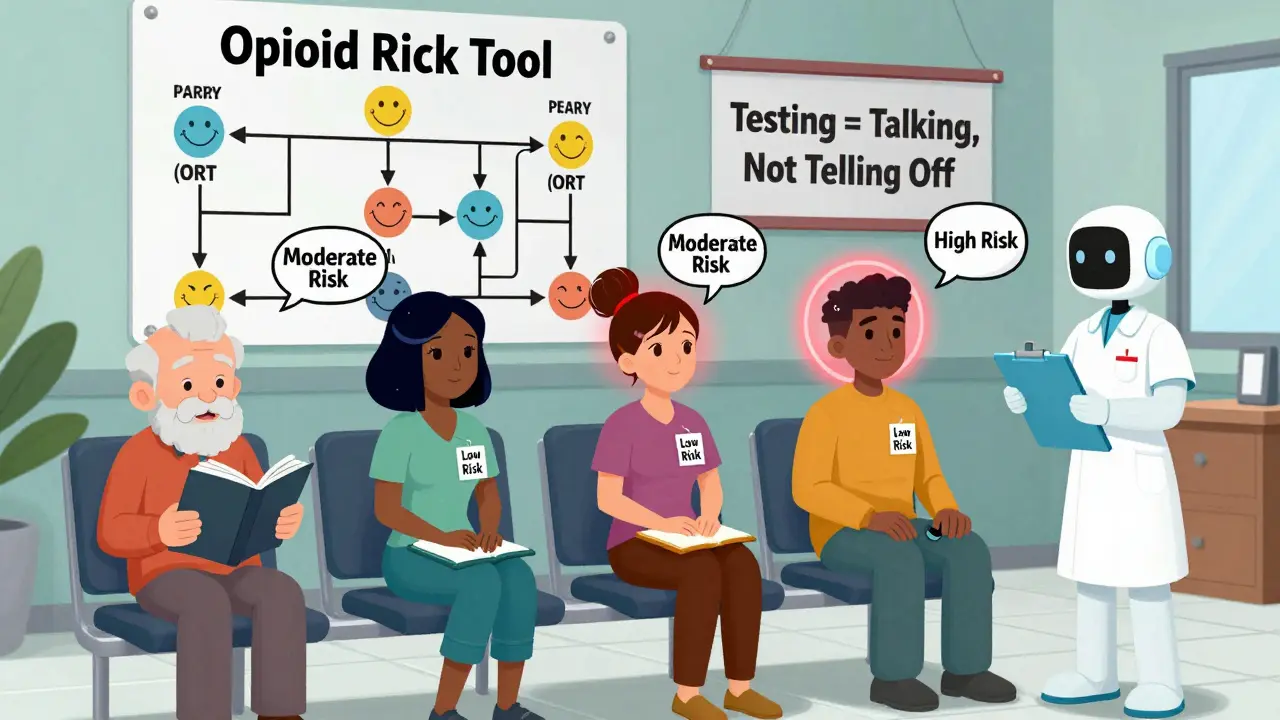
What’s Changing in 2025
The field is evolving fast. New FDA-approved tests now detect fentanyl reliably. The CDC is updating its guidelines expected in late 2024 to push for LC-MS testing for anyone on synthetic opioids. The American Medical Association now recommends testing frequency based strictly on ORT risk scores-not blanket policies. Point-of-care devices are coming. In 2025, some clinics will have machines that give lab-quality results in under an hour-right in the exam room. And AI tools are being tested to predict who’s likely to misuse opioids based on behavior patterns, not just urine results. But the biggest change? Shifting from punishment to partnership. The best clinics now treat negative tests as a conversation starter, not a red flag. “Tell me what happened,” becomes the new standard.What Patients Should Know
If you’re on opioids:- Ask what kind of test they’re using. Is it just a screen, or will they confirm with GC/MS if needed?
- Ask if they test for fentanyl and hydrocodone specifically.
- Bring a list of all medications-even OTC ones.
- Don’t assume a negative result means you’re in trouble. Ask for clarification.
- Know your risk level. If you’re low-risk, you shouldn’t be tested every month.
What Clinicians Should Do Differently
If you’re prescribing opioids:- Use the Opioid Risk Tool to set testing frequency-not guesswork.
- Always use fentanyl-specific or LC-MS testing for patients on synthetic opioids.
- Confirm positive or negative immunoassay results before taking action.
- Don’t use quantitative levels to judge dose compliance.
- Train your staff to interpret results correctly. A 2023 study found 40% of nurses misread basic test results.
- Make testing a collaborative step, not a punishment.
Are urine drug screens mandatory for opioid patients?
No, they’re not legally required everywhere, but 38 U.S. states mandate them for patients on high-dose or long-term opioid therapy. In the U.K., they’re recommended by guidelines but not enforced by law. Most reputable clinics use them as standard practice because they improve safety and reduce liability.
Can I be penalized for a false positive on a urine drug test?
Yes, unfortunately. Many patients have had prescriptions revoked or been labeled as “non-compliant” after false positives from over-the-counter meds or outdated test panels. Always ask for confirmatory testing if your result seems wrong. You have the right to request a second test using GC/MS or LC-MS.
Why does my hydrocodone show up as negative on my urine test?
Standard opiate immunoassays are designed to detect morphine, not hydrocodone. Up to 72% of patients taking hydrocodone test negative on these screens because the test doesn’t recognize the metabolite. You need a hydrocodone-specific test or LC-MS confirmation to get an accurate result. Tell your doctor if this keeps happening.
How often should I be tested if I’m on long-term opioids?
It depends on your risk level. Low-risk patients (no history of substance use, stable mental health) should be tested once a year. Moderate-risk patients (past substance use or mental health conditions) every six months. High-risk patients (active addiction, multiple risk factors) every three months-with validity checks for dilution or substitution.
Can I refuse a urine drug test?
Yes, you can refuse. But your doctor may choose to stop prescribing opioids if you refuse monitoring. This isn’t punishment-it’s a safety policy. Opioids carry serious risks, and without monitoring, doctors can’t safely manage them. If you’re uncomfortable with testing, talk to your provider about alternatives like extended-release formulations or non-opioid treatments.




