For years, parents were told to wait until their child was two or three before introducing peanut butter. That advice was everywhere - from pediatricians’ offices to baby books. But today, that old guidance has been completely flipped. Peanut allergy prevention isn’t about waiting anymore. It’s about acting early - and the science behind it is overwhelming.
In the U.S., about 2.2% of kids had peanut allergies in 2015. By 2023, that number dropped to 1.6%. That’s 300,000 fewer children with a life-threatening condition. Why? Because we stopped delaying and started introducing peanuts at the right time. The change didn’t come from guesswork. It came from a landmark study called LEAP, published in 2015, that changed everything.
What Changed? The LEAP Study That Rewrote the Rules
Before 2015, doctors told parents of babies with eczema or egg allergies to avoid peanuts. The thinking was simple: if your child is prone to allergies, don’t give them the most common trigger. But the number of peanut allergies kept rising. By 2010, it had doubled since 1997. Something was wrong.
The LEAP study, led by Dr. Gideon Lack at King’s College London, tested a bold idea: What if we gave peanut to high-risk babies early? They enrolled over 600 infants between 4 and 11 months old, all with severe eczema or egg allergy - the highest risk group. Half were told to avoid peanuts entirely. The other half got 2 grams of peanut protein, three times a week, for over three years.
The results? At age five, only 1.9% of the group that ate peanut developed an allergy. In the avoidance group? 13.7%. That’s a 86% drop in allergy risk. The study didn’t just show a trend - it proved prevention was possible. And it wasn’t a fluke. Later studies like EAT confirmed it: early exposure works.
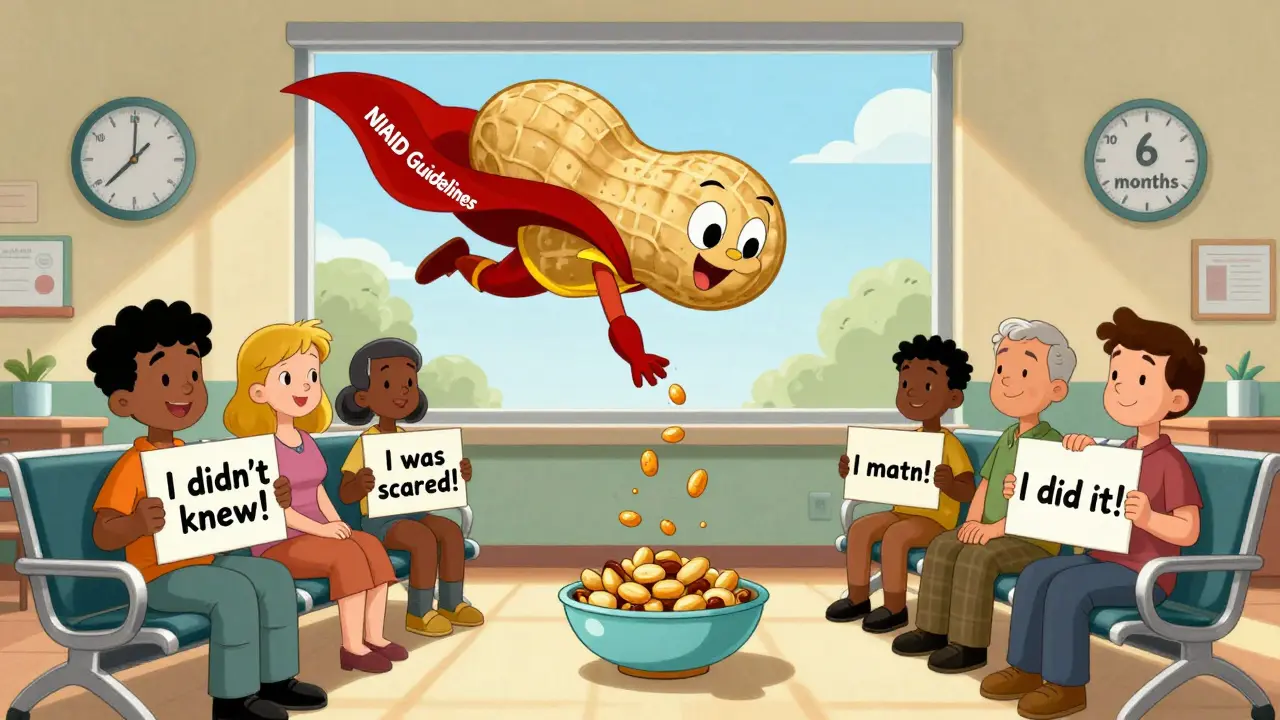
How to Introduce Peanut Based on Risk Level
Today, the National Institute of Allergy and Infectious Diseases (NIAID) gives clear, step-by-step guidance based on a baby’s risk level. It’s not one-size-fits-all. Here’s how it breaks down:
- High-risk infants (severe eczema or egg allergy): Start between 4 and 6 months. First, see a pediatrician. They may refer you to an allergist for a skin or blood test. If the test is negative, you can start giving peanut at home - but many doctors recommend the first dose be given in the clinic just to be safe. The goal: 2 grams of peanut protein, three times a week. That’s about 2 teaspoons of smooth peanut butter mixed into warm water, breast milk, or infant cereal. Never give whole peanuts or chunky peanut butter - choking risk.
- Moderate-risk infants (mild to moderate eczema): Start around 6 months at home. No testing needed. Just mix peanut into food and watch for reactions. If your baby tolerates it, keep giving it regularly.
- Low-risk infants (no eczema or food allergies): Introduce peanut anytime after starting solids, usually around 6 months. No special steps. Just make sure it’s in a safe form - smooth, diluted, mixed into food.
Why does timing matter so much? The data shows the earlier, the better. A 2023 meta-analysis found that babies who started peanut before 6 months had up to a 98% lower chance of developing an allergy. Even among babies with mild eczema, early introduction cut risk by 85%. The window is narrow - and closing fast.

Oral Immunotherapy (OIT) Is Not Prevention - It’s Treatment
Many people confuse early introduction with Oral Immunotherapy (OIT). They’re not the same. OIT is for kids who already have a peanut allergy. It’s a treatment, not a prevention strategy.
In OIT, a child with a confirmed peanut allergy eats tiny, increasing amounts of peanut protein under strict medical supervision. The goal isn’t to prevent allergy - it’s to build tolerance so they won’t have a severe reaction if they accidentally eat peanut. It takes months. It’s not risk-free. Some kids have reactions during treatment. It doesn’t cure the allergy. It just makes reactions less dangerous.
Early introduction is different. It’s for healthy babies - even those with eczema - who haven’t been diagnosed with an allergy yet. It’s about training the immune system early to see peanut as safe. And the effect lasts. Follow-up studies from LEAP showed that even after a year of avoiding peanut, kids who ate it early still didn’t develop allergies. That’s not just desensitization - it’s real tolerance.
Why So Many Parents Still Don’t Do It
Even with clear guidelines, only about 39% of high-risk infants in the U.S. are getting peanut early. Why? Three big reasons:
- Parental fear. A 2022 survey found 62% of parents were anxious about giving peanut to their baby. They worry about choking, vomiting, or anaphylaxis. But the risk of a reaction during supervised introduction is extremely low - far lower than the risk of developing a lifelong allergy.
- Confusion about how to do it. Many parents don’t know how to prepare peanut safely. They think peanut butter straight from the jar is okay. It’s not. Whole peanuts? Deadly. Chunky peanut butter? Risky. The right way: smooth peanut butter mixed with water, breast milk, or formula. Or use infant peanut puff snacks like Bamba - soft, dissolvable, and safe.
- Inconsistent advice from doctors. A 2023 survey found only 54% of pediatricians knew the current guidelines. Some still tell parents to wait. Others don’t mention peanut at all. If your pediatrician doesn’t bring it up, ask. Don’t assume they know.
There’s also a big equity gap. Black and Hispanic infants are 22% less likely to get early peanut introduction than White infants. That’s not just a statistic - it’s a health disparity that’s keeping allergy rates higher in those communities.
What Works - and What Doesn’t
Let’s cut through the noise. There are a lot of theories out there about preventing food allergies:
- Maternal diet during pregnancy? No strong evidence. Avoiding peanut while pregnant doesn’t help.
- Probiotics? Cochrane reviews found no benefit.
- Vitamin D supplements? No proven effect.
- Early introduction of multiple allergens? Yes. The EAT study showed that introducing peanut, egg, milk, and other allergens together at 3-4 months also reduced allergy rates. But peanut remains the most powerful single intervention.
Bottom line: The only strategy with consistent, strong, real-world evidence is early peanut introduction. No other method comes close.
The Future: What’s Next?
Research is moving fast. The PRESTO trial, funded by NIAID and running right now, is testing whether even lower doses of peanut protein - as little as 0.1 grams per week - can still prevent allergies. Results are expected in late 2026.
Meanwhile, the food industry is catching up. Products like spoonable peanut butter pouches and infant peanut puffs are growing 27% a year. More parents are finding safe, easy ways to give peanut. But access isn’t equal. In low-income areas, these products can be expensive or hard to find.
And long-term? The LEAP study showed protection lasting at least five years. If this holds, we could see peanut allergy become rare - not common - by 2030. GlobalData predicts prevalence could drop to 1.2% if early introduction rates climb from 39% to 65%.
The message is clear: Don’t wait. Don’t assume. If your baby has eczema or an egg allergy, talk to your doctor now. If they’re healthy, start peanut around 6 months. It’s not risky - it’s the safest thing you can do.
Can I give my baby peanut butter straight from the jar?
No. Whole peanuts, chunky peanut butter, or thick globs of peanut butter are choking hazards for babies. Always use smooth peanut butter mixed with water, breast milk, or formula to make it thin and safe. Or use infant-safe peanut puff snacks like Bamba.
Is it too late if my child is already one year old?
The best time is between 4 and 6 months, but it’s not too late. Even introducing peanut between 6 and 12 months still lowers allergy risk. The protective effect weakens after 12 months, but it’s still better than never introducing it. Talk to your pediatrician - they can help you decide what’s safe.
Do I need to test my baby before giving peanut?
Only if your baby is high-risk (severe eczema or egg allergy). For those babies, testing is recommended before introduction. For moderate or low-risk babies, no testing is needed. Just introduce peanut at home and watch for signs of a reaction - hives, vomiting, swelling, or trouble breathing. If any appear, stop and call your doctor.
What if my baby has a reaction during introduction?
If you see mild symptoms like a few hives or a rash, stop giving peanut and contact your pediatrician. If there’s swelling of the lips, tongue, or face, vomiting, wheezing, or trouble breathing - call emergency services immediately. These are signs of anaphylaxis. Always have an epinephrine auto-injector on hand if your baby is high-risk and you’re introducing peanut at home.
Does breastfeeding prevent peanut allergy?
No. Breastfeeding is healthy, but it doesn’t prevent peanut allergy. The only proven method is actively introducing peanut-containing foods to your baby between 4 and 6 months. What you eat while breastfeeding has no significant effect on allergy risk.