When your kidneys fail, dialysis isn’t just a medical procedure - it becomes part of your daily life. For many, doing it at home is the only way to keep working, traveling, or simply sleeping through the night. Two main types of home peritoneal dialysis exist: CAPD and APD. Choosing between them isn’t about which is better overall - it’s about which fits your body, your schedule, and your home.
What Is Peritoneal Dialysis?
Peritoneal dialysis uses the lining of your abdomen - the peritoneum - as a natural filter. A soft tube (catheter) is placed in your belly during a simple surgery. Dialysis fluid flows in through the tube, pulls waste and extra fluid out of your blood, then drains out. It’s done at home, without needles or a large machine like hemodialysis. This method gives you more control over your treatment schedule and avoids the stress of frequent trips to a clinic.
There are two ways to do it: manually, or with a machine. That’s where CAPD and APD come in.
CAPD: Manual Exchanges During the Day
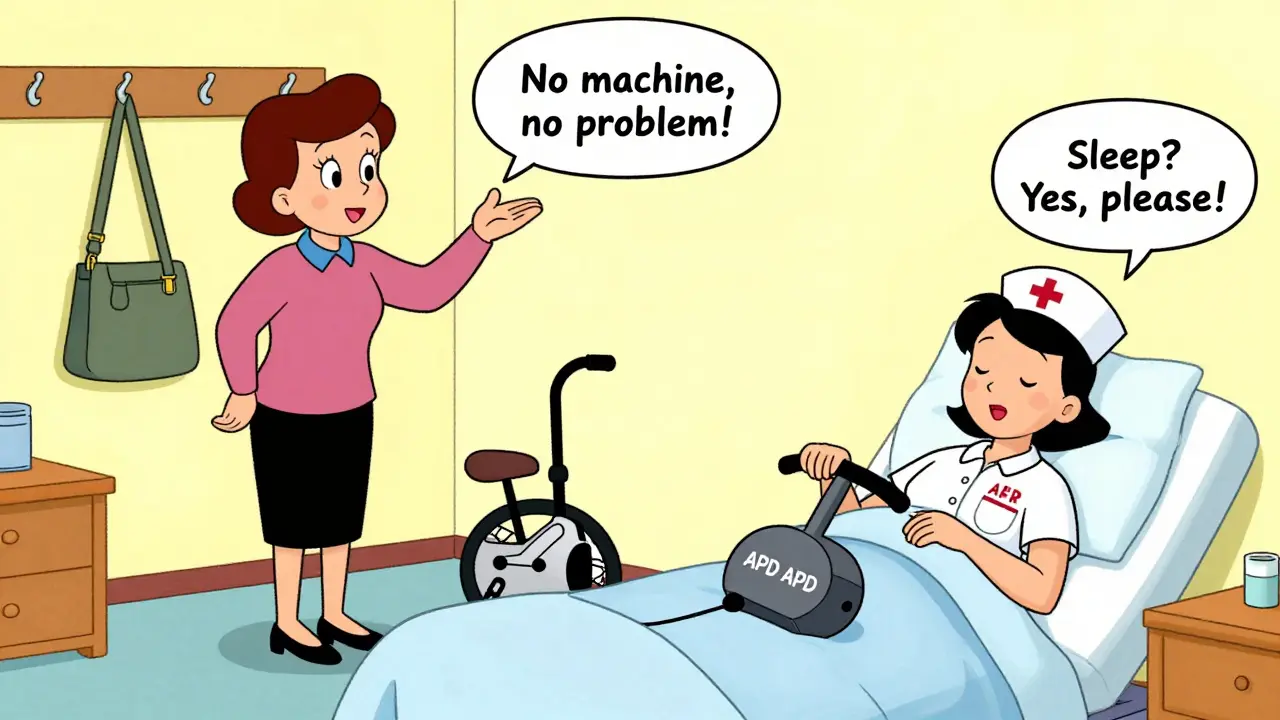
Continuous Ambulatory Peritoneal Dialysis (CAPD) means you do the exchanges yourself, by hand, during the day. No machine. No electricity. Just gravity.
You’ll do 3 to 5 exchanges every 24 hours. Each one takes about 30 to 40 minutes. You fill your belly with 1.5 to 3 liters of fluid, let it sit for 4 to 6 hours (this is called the dwell), then drain it out. You can walk around, eat, or even work while the fluid is in. Many people do exchanges during breaks - at lunch, after dinner, or before bed.
Because there’s no machine, you carry the fluid bags with you. Each bag weighs about 1.5 to 2 pounds. You’ll need space to store them - a closet or shelf near your bathroom works. You also need a clean, quiet place to do each exchange. A bathroom is ideal. You’ll need to wash your hands, wear a mask, and avoid dust or pets during the process.
Advantages? You’re not tied to a machine. You can travel easily. You don’t need an outlet. You’re in full control. Many people who work, teach, or have active lifestyles prefer CAPD because they can fit it into their routine.
But it’s not easy. Doing 4 or 5 exchanges a day, every day, means constant interruptions. If you’re on your feet all day, carrying bags can get tiring. And every time you connect or disconnect the tube, there’s a risk of infection. About 0.68 cases of peritonitis happen per patient each year with CAPD - higher than APD.
APD: Nighttime Treatment With a Machine
Automated Peritoneal Dialysis (APD) uses a machine - called a cycler - that does the exchanges for you while you sleep. You set it up before bed, and it runs for 8 to 10 hours. In the morning, you disconnect, drain the last bag, and go about your day.
Modern cyclers - like Baxter’s Amia, Fresenius’s Sleep-Safe, or HomeChoice - are quiet, compact, and weigh between 15 and 25 pounds. They need a power outlet and about 2x2 feet of floor space. Most have safety features: they detect air bubbles, monitor pressure, and shut down if something goes wrong. Some even send data to your care team remotely.
Because it’s done overnight, your days are free. No more stopping for dialysis at lunch. No carrying bags. You sleep through treatment. Studies show APD users get about 3.2 more hours of sleep per night than CAPD users. That matters - sleep improves mood, energy, and even how well your body handles fluid balance.
APD also gives better control over fluid removal. It’s more consistent. That means fewer spikes in blood pressure and less risk of fluid overload. A 2021 meta-analysis found APD users had 22% fewer hypertension emergencies than CAPD users.
But there are downsides. If the machine breaks - which happens to about 12% of users each year - you’re stuck. You might need emergency help. You can’t just grab a bag and go. You also need reliable electricity. Power outages can be dangerous. And if you’re a light sleeper, even a quiet cycler (35-45 decibels - like a library) can disturb your rest. About 19% of people who start APD stop because of noise or machine issues.
Which One Is Right for You?
There’s no single answer. It depends on your life, your health, and your home.
Choose CAPD if:
- You’re active during the day and want to avoid nighttime machines
- You travel often or live in an area with unreliable power
- You’re over 75 and prefer simple, manual tasks
- You have trouble sleeping or don’t want to be tied to a machine at night
- You’re comfortable with daily routines and don’t mind carrying bags
Choose APD if:
- You work full-time or have a busy daytime schedule
- You want more sleep and fewer interruptions during the day
- You have trouble with hand dexterity or find manual exchanges hard
- You have good electricity and space for a machine
- You’re under 65 and want the latest technology
For example, a 58-year-old teacher might pick CAPD because they can do exchanges during planning periods. A 42-year-old ER nurse might choose APD because they work 12-hour shifts and need to sleep uninterrupted.

Cost, Training, and Support
Medicare covers 80% of home dialysis costs in the U.S. Out-of-pocket expenses are lower for CAPD - about $50 to $75 a month for supplies. APD costs $75 to $100 a month because you’re renting the cycler. But APD can save money long-term: better fluid control means fewer hospital visits for heart or fluid problems. One study found APD users had 18% fewer hospitalizations.
Training takes longer for APD - 14 to 21 days - because you have to learn how to use, clean, and troubleshoot the machine. CAPD training is shorter - 10 to 14 days - but requires mastering sterile technique every single time. Both need a clean, dedicated space. APD needs an outlet. CAPD needs storage for bags.
Support is better for APD. Nearly all APD programs offer 24/7 tech help. Only 82% of CAPD programs do. And 78% of APD systems now send data to your nurse automatically - so if something’s off, they can call you before you get sick.
Real People, Real Choices
On patient forums, CAPD users say: “I love that I can do it anywhere - no machine, no wires.” But they also say: “I’m tired of stopping every few hours.”
APD users say: “I sleep through treatment. I don’t think about it until morning.” But they also say: “My cycler broke last month. I had to rush to the clinic.”
One survey of 1,200 home dialysis patients found CAPD users were 22% happier about travel flexibility. But APD users were 17% happier about sleep quality.
There’s no perfect choice. Only the right one for you.
What’s Changing in 2026?
Technology is moving fast. New APD machines now use AI to adjust fluid removal based on your weight and blood pressure. Baxter’s Amia system, launched in 2021, cut fluid overload events by 31% in trials. By 2025, the first smartphone-connected cycler will be FDA-approved - reducing setup errors by 40%.
Meanwhile, CAPD isn’t disappearing. It’s still the go-to for older patients, people in rural areas, and those without reliable power. But adoption is shifting. In 2023, APD made up 55% of home PD cases. By 2030, that’s expected to rise to 65%.
Doctors now recommend APD as a first option for most patients under 65 - if they have the space and support. But CAPD remains essential for those who can’t use machines.
What to Ask Your Doctor
Before you decide, ask:
- Do I have enough space at home for a machine or dialysis supplies?
- Is my power supply reliable? What happens during an outage?
- Can I manage sterile technique daily, or would a machine be safer?
- Do I have help at night if the cycler fails?
- What’s the backup plan if I can’t do my exchanges?
- Does my insurance cover both options fully?
Your doctor should help you test both methods during training. Try a few days of CAPD. Try a night on APD. See how you feel. Your body will tell you what works.
Final Thoughts
Peritoneal dialysis at home gives you freedom - but it also demands responsibility. CAPD gives you flexibility during the day. APD gives you freedom at night. One isn’t better. One is just better for you.
Most people who try home dialysis stay on it for years. The key isn’t picking the most advanced machine. It’s picking the one you can live with - day after day, year after year.
Can I switch from CAPD to APD later?
Yes. Many people start with CAPD and switch to APD if they want more sleep or find manual exchanges too tiring. Switching requires training on the cycler, but your care team will guide you. The catheter stays in place - you just change how you use it.
Is one method safer than the other?
Both are safe when done correctly. CAPD has a slightly higher risk of peritonitis because of more manual handling. APD reduces that risk with automated, sterile connections - but introduces risks like machine failure or power outages. Neither is risk-free. The key is training, hygiene, and having a backup plan.
Can I travel with APD?
Yes, but it’s harder than CAPD. You’ll need to ship dialysis fluid ahead, find outlets, and carry the cycler. Some cyclers are portable, but they still need power. Many APD users plan trips around hotel stays with outlets. CAPD is simpler - just pack bags and go.
What if I can’t afford the cycler?
Medicare and most private insurers cover cycler rental. If you’re underinsured, nonprofit groups like the American Kidney Fund help with equipment costs. CAPD is cheaper upfront, so it’s often the fallback option for those with financial limits.
Does age matter when choosing CAPD or APD?
Age plays a role. People over 75 often do better with CAPD because it doesn’t require learning complex machines. Younger patients under 65 usually prefer APD for the sleep benefits and fewer daytime disruptions. But it’s not just age - it’s dexterity, cognitive ability, and home support too.
How do I know if I’m a good candidate for home dialysis?
You need good vision, hand coordination, and a clean, quiet space. You should be motivated and have someone nearby who can help in an emergency. Your doctor will check your heart, abdomen, and mental health. If you can’t manage the routine safely, in-center dialysis might be better - even if it’s less convenient.
What’s Next?
If you’re considering home dialysis, start with a training session. Try both methods. Talk to people who’ve done it for years. Don’t rush. This isn’t a one-time decision - it’s a lifestyle. And the best choice is the one you can stick with for the long haul.



