Medication Safety Assessment Tool
How to Use This Tool
This tool assesses your symptoms against clinical guidelines to help you determine the right action for your medication.
Important: This is not a substitute for medical advice. Always consult your healthcare provider.
Not every side effect means you should stop your medication. In fact, stopping the wrong drug at the wrong time can be more dangerous than the side effect itself. Every year, over 1.3 million people in the U.S. end up in the emergency room because of adverse drug reactions. But here’s the twist: nearly 20% of those cases happen because someone stopped a medication too quickly - without realizing they were trading one risk for a worse one.
When to Stop Right Away
Some side effects aren’t just uncomfortable - they’re life-threatening. If you experience any of these, stop the medication immediately and get medical help:- Anaphylaxis: Swelling of the throat, trouble breathing, hives, rapid pulse, or a sudden drop in blood pressure. This can happen within minutes of taking a drug. Penicillin is the most common cause, but any medication can trigger it. About 1 in 10,000 people will have this reaction.
- Stevens-Johnson Syndrome (SJS) or Toxic Epidermal Necrolysis (TEN): A blistering, painful rash that spreads and causes skin to peel off like a burn. It often starts with flu-like symptoms, then a red or purple rash that turns into blisters. Medications like carbamazepine, lamotrigine, allopurinol, and sulfa drugs are frequent culprits. SJS has a 5-15% death rate. TEN kills up to half the people who get it.
- Acute liver failure: Yellowing skin or eyes, dark urine, severe nausea, vomiting, or confusion. If your liver enzymes (ALT) are more than 3 times the normal level and you have symptoms - or 5 times higher even without symptoms - stop the drug. Isoniazid, used for tuberculosis, causes this in about 1 out of 10,000 people.
- Agranulocytosis: A sudden, dangerous drop in white blood cells. You’ll feel extremely tired, get fevers, and develop mouth sores or infections that won’t heal. This happens in 1-15 out of every million users of drugs like clozapine or antithyroid medications. Without stopping the drug, death rates hit 5-10%.
These reactions don’t wait. They don’t improve with time. If you see them, don’t wait for your next appointment. Call 911 or go to the ER.
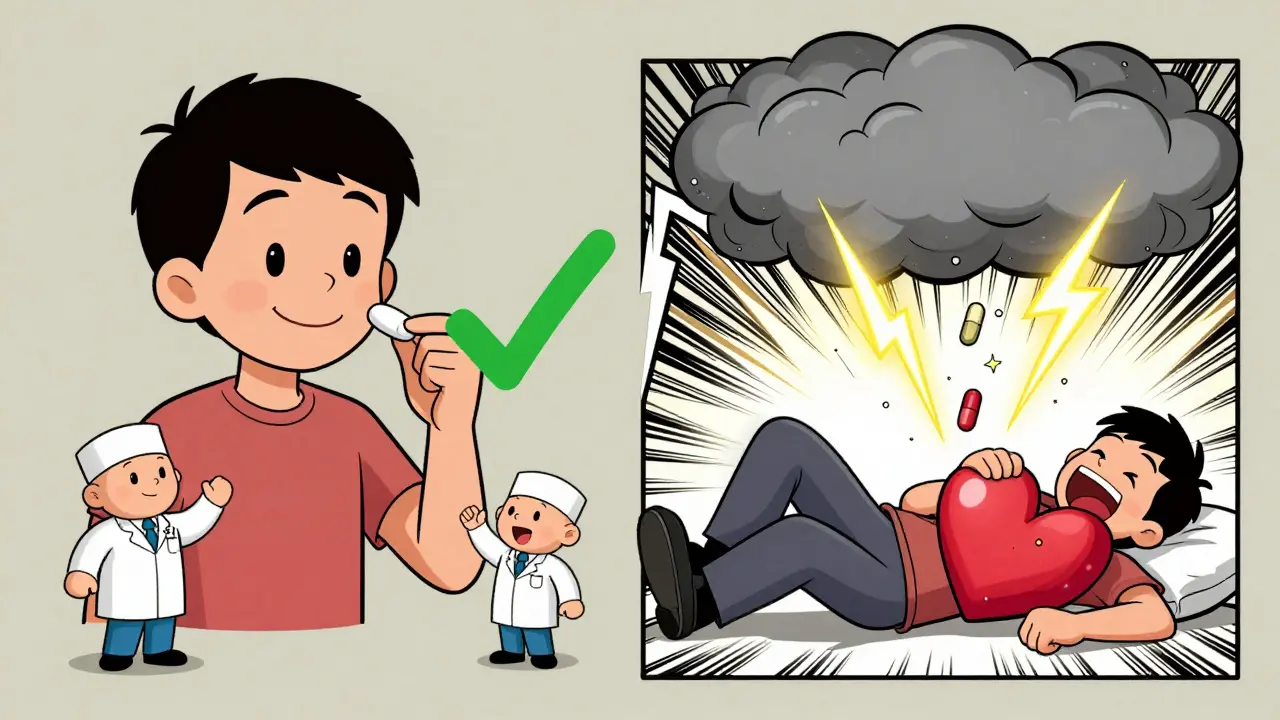
Why Stopping Too Soon Can Kill You
Many medications are safe to keep taking even if they cause nausea, dizziness, or a rash - as long as it’s mild. But some drugs, if stopped suddenly, can trigger emergencies worse than the side effect you’re trying to escape.- Beta blockers (like metoprolol or propranolol): Stopping these cold turkey can spike your heart rate and blood pressure. In people with heart disease, this raises the risk of a heart attack by 300% in the first week.
- Benzodiazepines (like Xanax or Valium): Abruptly quitting can cause seizures, hallucinations, or extreme anxiety. About 10-15% of long-term users have withdrawal seizures if they stop without tapering.
- Antidepressants: Even SSRIs like sertraline or fluoxetine can cause discontinuation syndrome - dizziness, brain zaps, nausea, insomnia - in 20-50% of people. But these aren’t life-threatening. Stopping them suddenly won’t kill you, but it can make you feel awful for weeks.
- Clonidine (for high blood pressure): Stopping it suddenly can cause your blood pressure to skyrocket. Some patients end up in hypertensive crisis - a medical emergency.
These aren’t myths. They’re backed by data. The American College of Physicians found that over 65% of all bad outcomes from stopping meds come from just two groups: cardiovascular drugs and CNS depressants. You don’t fix one problem by creating another.
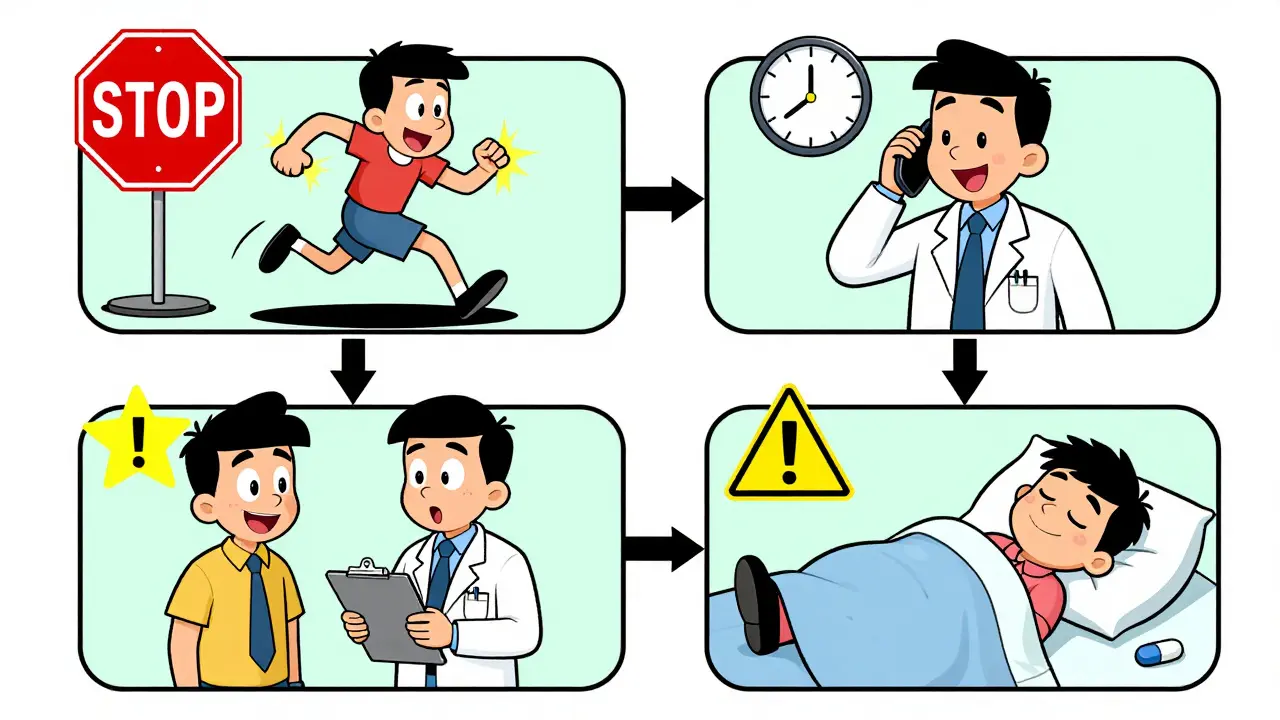
The Four-Tier Rule: How Doctors Decide
There’s no one-size-fits-all answer. That’s why experts use a simple four-tier system to decide what to do:- Tier 1: Stop Immediately - Anaphylaxis, SJS/TEN, acute liver failure, agranulocytosis. No delay. No second opinion needed.
- Tier 2: Stop Within 24-48 Hours - Severe skin rashes without blistering, major kidney or liver damage that’s worsening, or signs of severe infection linked to the drug.
- Tier 3: Talk to Your Doctor Before Stopping - Nausea, dizziness, mild rash, fatigue, or headaches that last more than a week. These are often temporary. A dose change or switch to another drug might help.
- Tier 4: Keep Taking It - Mild, short-lived side effects like dry mouth, slight weight gain, or trouble sleeping. These often fade in a few days or weeks.
Doctors don’t guess. They use this system. And if you’re unsure where your side effect falls, don’t assume. Ask.
What Patients Get Wrong
A 2022 study found that 31% of people stopped statins because of muscle pain - but only 5% of those cases were true statin-induced myopathy. The rest? Likely unrelated. Maybe they were dehydrated. Maybe they started a new workout. Maybe it was aging. But they quit anyway.On Reddit, one user wrote: “I stopped my antidepressant cold turkey after feeling weird. Now I’m worse than before.” Over 200 comments replied: “You didn’t need to stop. You needed to talk to your doctor.”
Here’s the truth: 42% of patients stop medications because of side effects - without telling anyone. And 18% of those people end up with worse health problems because of it.
And it’s not just about stopping. It’s about how you stop. The FDA now requires all SSRIs to include specific tapering schedules on their labels. Why? Because when people slowly reduce their dose over weeks instead of quitting cold turkey, the risk of withdrawal symptoms drops by 73%.
What You Should Do
Here’s your action plan:- Know your meds. If you’re on any of these - beta blockers, benzodiazepines, antidepressants, clonidine, steroids - don’t stop without talking to your provider.
- Track your symptoms. Write down when the side effect started, how bad it is (1-10 scale), and if it’s getting worse or better. This helps your doctor decide faster.
- Don’t Google and decide. A rash might be harmless. Or it might be SJS. Only a doctor can tell the difference.
- Ask about alternatives. If a drug causes side effects, there’s often another one that doesn’t. For example, if you can’t tolerate one statin, another might work fine.
- Always refill your prescription. Running out of blood pressure or seizure meds can be deadly. Don’t let a pharmacy delay become an emergency.
Bottom Line
Side effects are common. But not all of them mean you should quit. The difference between life and danger isn’t always obvious. Anaphylaxis? Stop now. A headache from your blood pressure pill? Wait. Talk. Adjust. Don’t assume.Medications are powerful tools. But they’re not magic. They need respect - and smart decisions. The goal isn’t to avoid side effects at all costs. It’s to manage them safely so you stay healthy, not hospitalized.
Can I stop a medication if the side effect is annoying but not dangerous?
No, not without talking to your doctor first. Many side effects like nausea, dizziness, or fatigue are temporary and fade within days or weeks. Stopping a drug like a beta blocker or antidepressant suddenly can cause worse problems - like a spike in blood pressure or withdrawal seizures. Always ask your provider if there’s a safer way to manage the side effect, like lowering the dose or switching medications.
What should I do if I think I’m having an allergic reaction?
Stop the medication immediately and seek emergency care. Signs include swelling of the face, lips, or throat; trouble breathing; hives; or a sudden drop in blood pressure. Anaphylaxis can kill within minutes. Don’t wait to see if it gets better. Call 911 or go to the nearest ER. Bring the medication bottle with you.
Are all rashes from medications dangerous?
No. Many rashes are mild, itchy, and go away on their own. But if the rash spreads quickly, turns into blisters, involves your mouth or eyes, or is accompanied by fever or peeling skin, stop the drug and get help immediately. These could be signs of Stevens-Johnson Syndrome or toxic epidermal necrolysis - rare but deadly reactions.
Why do some drugs need to be tapered instead of stopped?
Your body adapts to long-term medications. Stopping suddenly can cause your system to go into shock. Beta blockers slow your heart - if you stop fast, your heart races dangerously. Benzodiazepines calm your brain - quit cold turkey, and your brain overfires, causing seizures. Tapering lets your body adjust slowly, avoiding these rebound effects.
Can I switch to a different medication if I have side effects?
Often, yes. Many side effects are drug-specific, not condition-specific. If one statin causes muscle pain, another might not. If one antidepressant makes you nauseous, a different class might work better. Talk to your doctor - don’t assume you have to live with the side effect. There are usually alternatives.
What if I accidentally stopped a medication and feel worse?
Call your doctor right away. If you stopped a blood pressure or heart medication, you could be at risk for a heart attack or stroke. If you stopped an antidepressant or anti-seizure drug, you might be heading into withdrawal. Don’t wait. Tell them exactly what you stopped, when, and how you’re feeling. They can guide you on whether to restart, taper, or switch.