Diagnosing Dyskinesias
Dyskinesias are involuntary, often jerky or writhing movements. They can be mild and barely noticeable or severe enough to affect walking, speaking, and daily tasks. Figuring out whether a movement is a dyskinesia — and what type — matters because treatment choices depend on the cause and timing.
Common signs and types
Watch for movements that you can't control, especially if they show a pattern with medication timing. Here are common types you might hear about:
- Peak‑dose dyskinesia: movements occur when medication (often levodopa) is at its strongest. They tend to be lively and repetitive.
- Diphasic dyskinesia: appears as medication levels rise or fall — usually at the start or end of a dose — and often affects the legs more.
- Dystonic dyskinesia: sustained muscle contractions that cause twisting or abnormal postures, sometimes painful.
- Tardive dyskinesia: chorea-like mouth, tongue, or facial movements that develop after long-term use of certain antipsychotics or other drugs. This is assessed differently than Parkinson's-related dyskinesias.
How doctors diagnose and what you can do
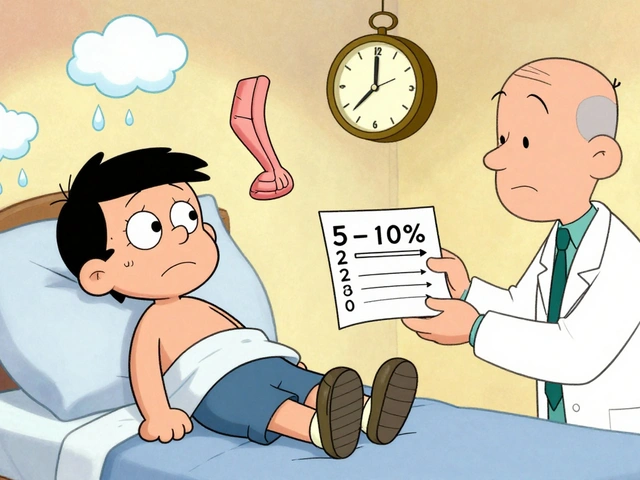
Diagnosis is mostly clinical: your doctor watches you move and asks detailed questions. Expect them to ask about medication names, doses, and exactly when movements start and stop relative to doses. They may use short rating tools—AIMS for tardive dyskinesia or parts of the UPDRS for Parkinson's-related movement—to document severity.
Bring a simple record to your visit: a one-week diary that notes the time of each medication dose and when symptoms appear or change. Short videos taken on a phone are extremely helpful. Record a few 30–60 second clips showing the movement at its worst and when it's minimal. Note activities, sleep, stress, and any new medicines or supplements.
Doctors also rule out look-alikes: tremor (rhythmic), chorea (random, flowing), myoclonus (sudden jerks), and tics (suppressible urges). The time link with meds often points to dyskinesia. If the cause is unclear, a neurologist or movement-disorder specialist may order more focused exams or recommend a medication trial, observation, or wearable motion sensors for detailed tracking.
When to see a specialist? If movements start suddenly, worsen quickly, cause falls, interfere with daily living, or appear after starting a new drug, get evaluated. If symptoms slowly reduce your quality of life, a specialist can review medication timing, try dose adjustments, add treatments like amantadine, or discuss advanced options such as deep brain stimulation in selected cases.
Quick checklist before your appointment: list of current meds with doses and times, short videos of the movements, notes on when they happen each day, and a brief note on how they affect your life. That information speeds up diagnosis and helps your clinician pick the right first step.