DKD Prevention: How to Stop Diabetic Kidney Disease Before It Starts
When you have diabetes, your kidneys are under constant stress. Diabetic kidney disease, also called diabetic nephropathy, is a progressive condition where high blood sugar damages the tiny filters in your kidneys. Also known as DKD, it’s the leading cause of kidney failure in the U.S.—and the good news is, it’s often preventable. Most people don’t feel symptoms until damage is advanced. That’s why DKD prevention isn’t about waiting for warning signs. It’s about acting early, consistently, and with clear goals.
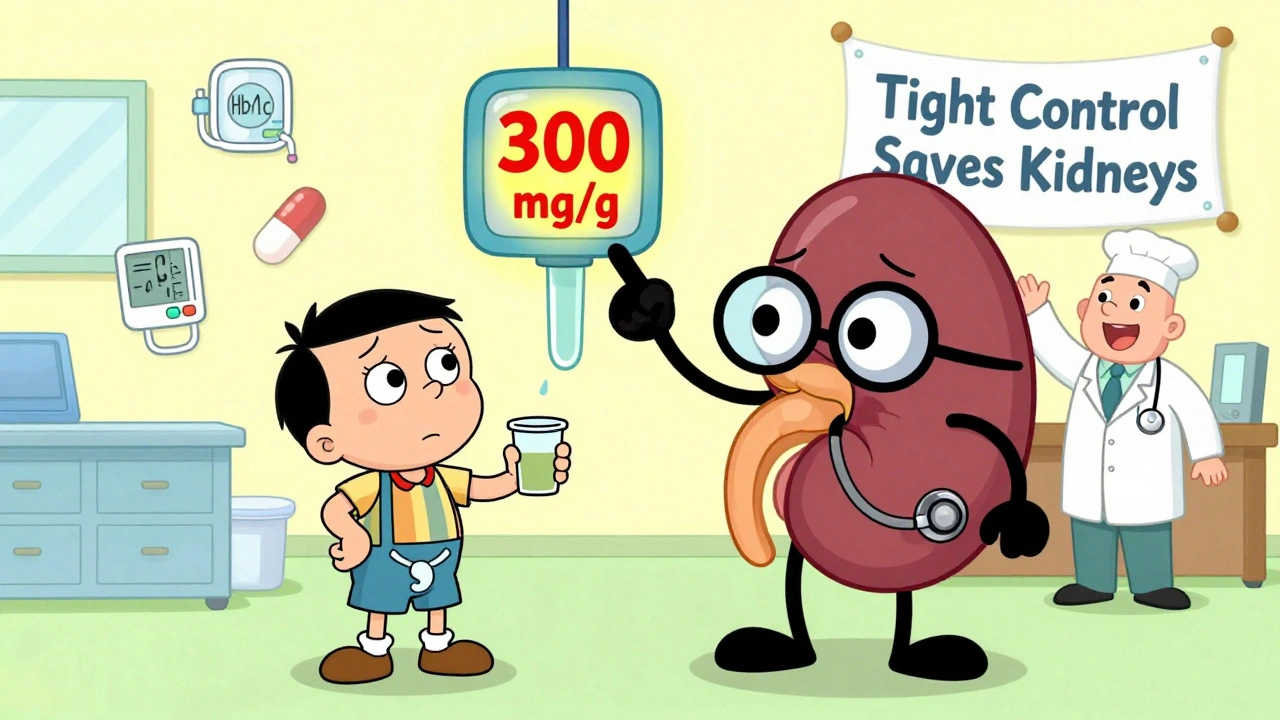
Chronic kidney disease, a broader term that includes DKD, affects over 37 million Americans. But not all cases come from diabetes. Diabetes management, the foundation of DKD prevention, means more than just checking your glucose. It’s about keeping HbA1c under 7%, managing blood pressure below 130/80, and avoiding NSAIDs like ibuprofen that strain your kidneys. Even small changes—like swapping soda for water, walking 30 minutes a day, or cutting back on salt—add up. Studies show that tight control can reduce kidney damage risk by up to 30%. Medications like SGLT2 inhibitors and GLP-1 agonists aren’t just for blood sugar—they’re now proven to protect your kidneys too. If you’re on these drugs, you’re already ahead.
Kidney health isn’t a one-time test. It’s tracked with annual urine albumin and eGFR tests. If your doctor skips these, ask. Many people with early DKD have no swelling, no fatigue, no pain. The damage happens silently. But catching it early means you can still turn things around. The posts below cover exactly how: from checking your medication list to spotting hidden risks from drugs like SGLT2 inhibitors, understanding why some side effects fade over time, and how to avoid drug interactions that hurt your kidneys. You’ll find real strategies—not theory—on how to protect your kidneys while managing diabetes, what to ask your pharmacist, and how to spot the warning signs before it’s too late.