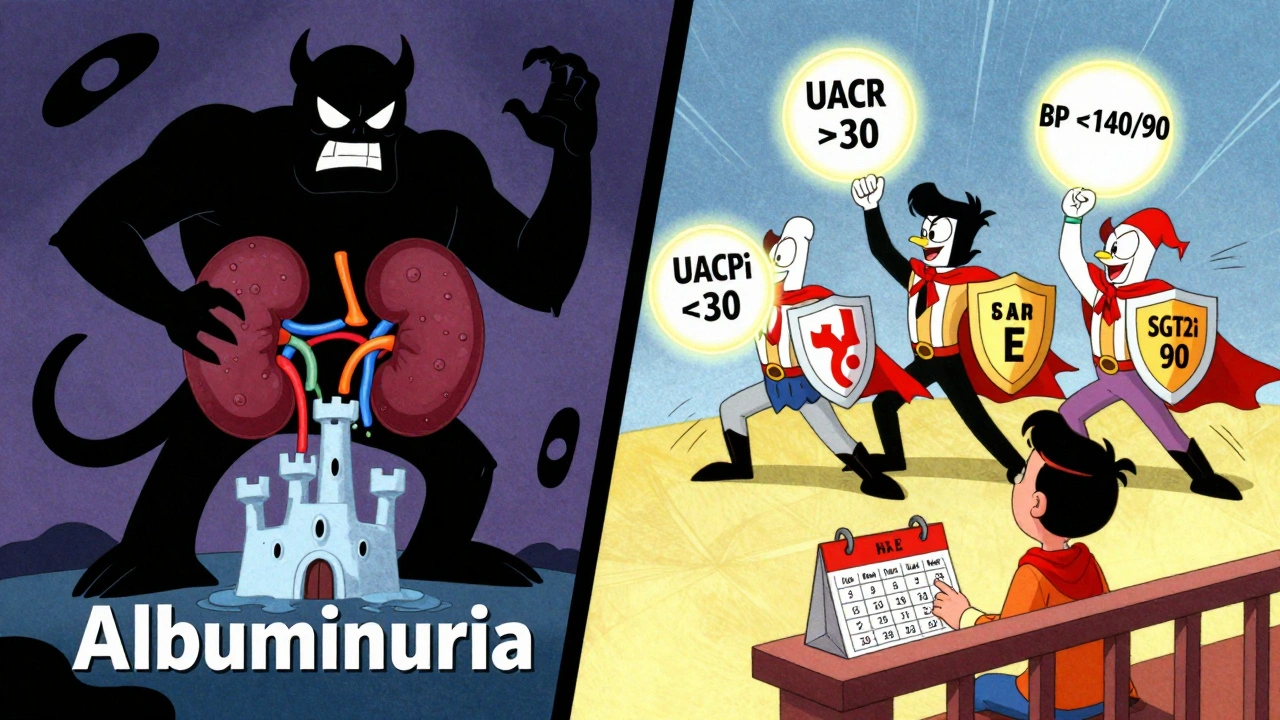
When your kidneys start leaking protein into your urine, it’s not just a lab result-it’s your body screaming for help. In people with diabetes, this early warning sign is called albuminuria, and it’s the first clear signal that diabetic kidney disease (DKD) is taking root. Left unchecked, it can lead to kidney failure, heart attacks, and early death. But here’s the good news: catching it early and acting fast can stop it in its tracks.
What Albuminuria Really Means
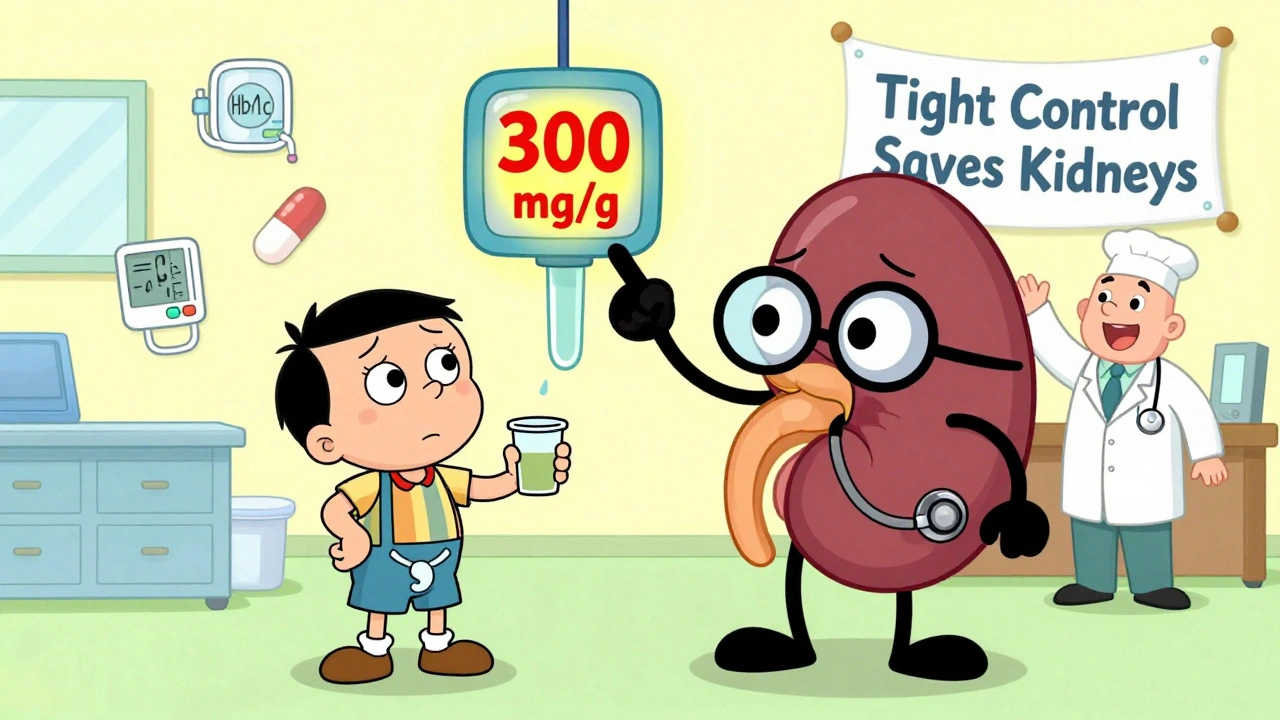
Albumin is a protein your kidneys normally keep inside your blood. When they start letting it slip into your urine, something’s wrong. That’s albuminuria. It’s not a disease itself-it’s a red flag. For decades, doctors called small amounts "microalbuminuria" and large amounts "macroalbuminuria." But in 2012, experts changed the names to make it simpler: normal (<30 mg/g), moderately increased (30-300 mg/g), and severely increased (>300 mg/g). The key takeaway? Any amount above 30 mg/g means kidney damage is happening.
This isn’t just theoretical. A study of over 128,000 diabetic patients found that those with albuminuria over 300 mg/g had a 73% higher risk of dying from any cause and an 81% higher risk of dying from heart disease. The higher the number, the worse the outlook. And here’s what makes it even more urgent: albuminuria often shows up years before your kidney function drops. By the time your eGFR (a measure of how well your kidneys filter blood) falls below 60, the damage is already advanced.
How Doctors Detect It
Testing for albuminuria is easy. You give a single urine sample-a spot test-and the lab measures how much albumin is in it compared to creatinine. That’s the UACR: Urine Albumin-to-Creatinine Ratio. It’s accurate, cheap, and done in minutes.
But one high result doesn’t mean you have DKD. Albuminuria can spike temporarily from things like intense exercise, a fever, uncontrolled blood sugar over 300 mg/dL, or even your period. That’s why guidelines say you need two out of three abnormal tests within 3 to 6 months to confirm the diagnosis. If your first test shows 250 mg/g, don’t panic. Retest in 3 months. If it’s still high, then it’s real.
Annual screening is the standard for everyone with type 2 diabetes at diagnosis and for those with type 1 diabetes after 5 years. Yet in real clinics, only about 60% of patients get tested each year. Why? Many doctors don’t have automated reminders in their systems. Patients forget to bring samples. Or they think, "If I feel fine, why test?" But DKD doesn’t cause symptoms until it’s too late. That’s why testing isn’t optional-it’s life-saving.
Tight Control Isn’t Just a Buzzword
"Tight control" sounds vague, but it’s simple: get your blood sugar as close to normal as safely possible. The landmark DCCT trial in the 1990s showed that type 1 diabetes patients who kept their HbA1c under 7% cut their risk of developing albuminuria by 39% and progression to proteinuria by 54%. Those benefits lasted for decades-even after they relaxed their control. That’s called "metabolic memory." Your body remembers good blood sugar control long after you stop chasing perfect numbers.
For type 2 diabetes, the UKPDS trial found that every 1% drop in HbA1c lowered the risk of kidney disease by 21%. Today, the American Diabetes Association recommends HbA1c under 7% for most people. If you’re young, healthy, and at low risk of low blood sugar, aiming for 6.5% can offer even more protection. But pushing too hard can be dangerous. Hypoglycemia can kill just as surely as high blood sugar. So work with your doctor to find your sweet spot.
Blood Pressure Matters Just as Much
High blood pressure and high blood sugar are a deadly team. Together, they crush your kidneys. The KDIGO guidelines say that if your albuminuria is over 300 mg/g, your blood pressure target should be under 120/80. But the SPRINT trial showed that pushing systolic pressure below 120 mmHg reduced albuminuria by 39%-but also increased the risk of sudden kidney injury in 1 out of every 47 people. So most guidelines, including the ADA, still recommend keeping blood pressure under 140/90 for most patients with DKD.
What’s not up for debate: if you have albuminuria, you need a blood pressure medication that protects your kidneys. That means ACE inhibitors or ARBs. These drugs don’t just lower pressure-they directly reduce protein leakage. The IRMA-2 trial proved that losartan, an ARB, cut the progression from moderate to severe albuminuria by 53%. The rule now? Start these drugs early and titrate them to the highest tolerated dose, even if your blood pressure is normal. That’s not off-label-it’s standard care.
The New Game-Changers: SGLT2 Inhibitors and Finerenone
For years, ACEi/ARBs were the only weapons. Now we have two more powerful tools.
First, SGLT2 inhibitors like empagliflozin. The EMPA-KIDNEY trial showed that in patients with DKD and albuminuria over 200 mg/g, empagliflozin cut the risk of kidney failure or death by 28%. It works by making your kidneys flush out sugar and salt-reducing pressure inside the filtering units. It also helps your heart. That’s why it’s now recommended as first-line therapy alongside ACEi/ARBs, even if you don’t have high blood sugar.
Then there’s finerenone, a newer drug that blocks a hormone called aldosterone. In trials, it reduced albuminuria by 32% in just 4 months and slowed kidney decline by 23% over three years-even in patients already on maximum ACEi/ARB therapy. It’s not for everyone, but if you have persistent albuminuria despite other treatments, your doctor should consider it.
Here’s the shocking part: only about 29% of people with DKD are actually getting all three recommended treatments-ACEi/ARB, SGLT2i, and finerenone if needed. Why? Cost, lack of awareness, and systemic gaps in care. In low-income communities, patients often can’t afford these meds or can’t get follow-ups. That’s why screening and treatment aren’t just medical issues-they’re social justice issues.
What You Can Do Right Now
If you have diabetes, here’s your action plan:
- Ask for your UACR test every year. Don’t wait for your doctor to bring it up.
- If your result is above 30 mg/g, get two more tests within six months to confirm.
- If confirmed, insist on an ACE inhibitor or ARB-even if your blood pressure is normal.
- Ask if an SGLT2 inhibitor like empagliflozin or dapagliflozin is right for you.
- Check your HbA1c every 3 months. Aim for under 7%, or lower if safe.
- Keep your blood pressure under 140/90. Use a home monitor if needed.
- Avoid NSAIDs like ibuprofen-they hurt kidneys in DKD.
- Stop smoking. It doubles your risk of kidney failure.
These steps aren’t optional. They’re the difference between living with kidney disease and living well.
Why This Matters More Than Ever
Diabetic kidney disease is the leading cause of kidney failure in the U.S. and the UK. But it’s also one of the most preventable. The 2024 ADA/KDIGO report estimates that if everyone followed current guidelines, we could prevent 1.2 million new cases of DKD in the U.S. alone by 2030. That’s 37% fewer people on dialysis. It’s $14.8 billion saved in healthcare costs.
But none of that happens without action-from patients, doctors, and the system. If you’re reading this, you might be one person who’s about to change that. Get tested. Ask questions. Demand better care. Your kidneys won’t tell you they’re failing until it’s too late. But this test? It’s your early warning system. Use it.
Can albuminuria go away?
Yes, in some cases. If caught early and treated aggressively with tight blood sugar control, ACE inhibitors or ARBs, and SGLT2 inhibitors, albuminuria can drop back into the normal range. Studies show that reducing UACR by more than 30% from its peak lowers the risk of kidney failure by nearly half. It’s not guaranteed, but it’s possible-and it’s worth fighting for.
Do I need a 24-hour urine test?
No. Spot urine tests (UACR) are now the standard. They’re just as accurate, much easier, and cheaper. A 24-hour collection is only used in rare cases, like when results are unclear or for research. Your doctor will order a spot test first.
Can I still drink alcohol with diabetic kidney disease?
Moderate alcohol (one drink per day for women, two for men) is usually okay if your diabetes and blood pressure are under control. But alcohol can raise blood pressure and interfere with medications. It can also mask low blood sugar symptoms. Talk to your doctor about your personal risk.
Is there a cure for diabetic kidney disease?
There’s no cure yet, but it can be halted or even reversed in early stages. The goal isn’t to cure-it’s to stop progression. With the right combination of medications, diet, and lifestyle changes, many people never progress beyond mild albuminuria. That’s the best outcome possible.
Why do I need to check my blood pressure at home?
Blood pressure can vary wildly in a doctor’s office due to stress. Home readings give a clearer picture of your real risk. If your home readings are consistently above 130/80, you need to adjust your treatment. Home monitoring is now a key part of managing DKD.
What foods should I avoid with albuminuria?
Cut back on processed foods, salt, and added sugars. High salt intake makes albuminuria worse and raises blood pressure. Avoid canned soups, deli meats, frozen meals, and sugary drinks. Focus on whole foods: vegetables, lean proteins, whole grains, and healthy fats. A dietitian can help you build a kidney-friendly meal plan.
Can I exercise with diabetic kidney disease?
Yes-exercise is one of the best things you can do. Regular activity improves insulin sensitivity, lowers blood pressure, and helps control weight. But avoid intense workouts right before a UACR test, as they can temporarily raise albumin levels. Aim for 30 minutes of walking, cycling, or swimming most days.
What happens if I skip my kidney meds?
Skipping ACE inhibitors, ARBs, SGLT2 inhibitors, or finerenone can cause albuminuria to rise again-and quickly. Each missed dose increases your risk of kidney damage and heart events. These aren’t optional pills-they’re protective shields. If cost or side effects are a problem, talk to your doctor. There are often solutions.
Next Steps: What to Do Today
If you have diabetes and haven’t had a UACR test in the last year, call your doctor now. Ask for the test. Bring your results to your next appointment and ask: "Is my albuminuria under control? What’s my next step?"
If you’ve been diagnosed with albuminuria, don’t wait. Start the conversation about ACEi/ARBs, SGLT2 inhibitors, and lifestyle changes. Ask if finerenone might help. Get a home blood pressure monitor. Track your numbers. Join a diabetes education program if one’s available.
Diabetic kidney disease doesn’t happen overnight. But it doesn’t stop on its own either. The window to act is wide open-right now. Use it.