Glaucoma treatment: Protect your vision now
Glaucoma is one of the fastest moving causes of permanent vision loss, but treatment often slows or stops damage when caught early. If you have high eye pressure or optic nerve changes, there are clear steps you can take now to lower risk. The goal of any plan is simple: stop nerve damage and preserve the vision you still have.
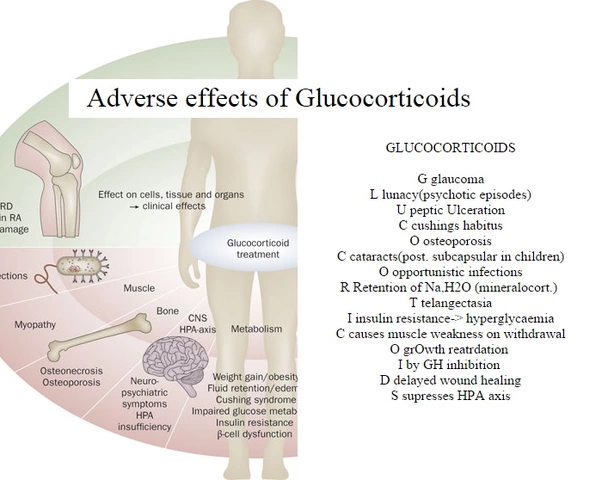
The first line of treatment is usually prescription eye drops. Drops lower eye pressure by either reducing fluid production or improving drainage. Common types include prostaglandin analogs, beta blockers, alpha agonists, carbonic anhydrase inhibitors, and rho kinase inhibitors. Side effects vary: some cause red eyes or eyelash growth, others may affect breathing or heart rate. Use them exactly as prescribed and bring a list of current meds to your doctor to avoid interactions.
Common treatments
If drops don't work or adherence is a problem, laser therapy is often next. Selective laser trabeculoplasty (SLT) can improve drainage with an outpatient office procedure that takes minutes. Many people see lower pressure for months or years. It doesn’t remove the need for follow-up checks.
When laser or drops aren’t enough, surgery can help. Traditional options include trabeculectomy and tube shunts that create new drainage paths. Newer minimally invasive glaucoma surgeries (MIGS) offer less recovery time and may suit early to moderate disease, especially during cataract surgery. Talk with your surgeon about likely risks and recovery timelines.
Lifestyle and monitoring
Small daily choices matter. Regular exercise (brisk walking or swimming) can lower eye pressure for some people. Avoid Valsalva maneuvers like heavy straining that spike pressure. Check with your doctor about caffeine intake; high doses can temporarily raise pressure. Wear protective eyewear to prevent trauma that could worsen glaucoma.
Follow-up matters more than any single treatment. You’ll need regular eye pressure checks, optic nerve photos, and visual field tests to track progress. If tests show worsening, don’t wait — ask about changing drops, adding laser, or referring to a glaucoma specialist.
Questions to ask your doctor: What is my target eye pressure? How often should I get visual field testing? What are the side effects of the drops you recommend? How long before I try laser or surgery? Will my other health conditions affect treatment choices?
Finally, manage expectations. Most treatments aim to slow progression rather than restore lost sight. With timely care, many people keep useful vision for life. If you notice new vision loss, sudden eye pain, or nausea with eye redness, get urgent care — some glaucoma types are medical emergencies.
If you want, bring a friend to appointments, keep a medication calendar, and use reminder apps to avoid missed doses. Good communication with your eye team and steady monitoring give you the best chance to protect your sight.
Ask about help with cost and generic options, and don’t hesitate to get a second opinion if your pressure stays high. Tracking apps and home tonometry are options some patients use under doctor guidance. Stay proactive.