Gouty arthritis: what it feels like and why it happens
Gouty arthritis can hit suddenly — often overnight — with a joint that becomes red, hot and so painful you can’t bear a sheet on it. Most people think of the big toe, but gout can affect ankles, knees, wrists, and fingers too. The pain comes from tiny monosodium urate crystals building up in the joint when blood uric acid is too high (usually above about 6.8 mg/dL).
What causes a gout attack?
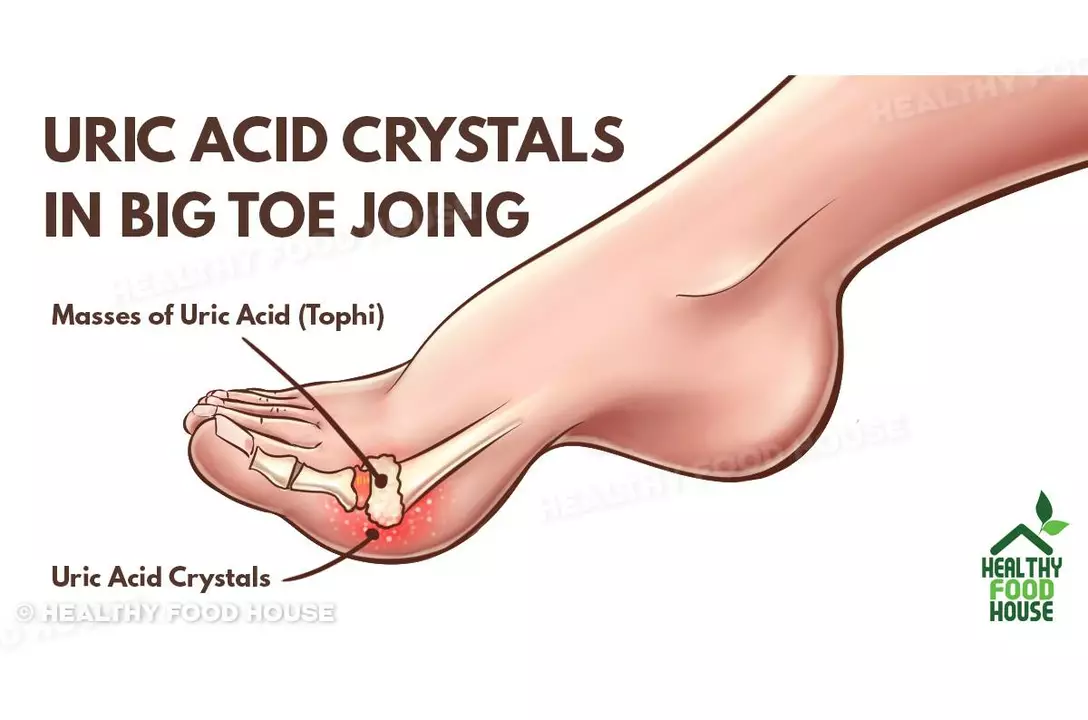
Uric acid is a normal breakdown product from certain foods and your body. When kidneys can’t clear it fast enough, crystals form and trigger inflammation. Triggers that often spark a flare: drinking beer or spirits, eating a lot of red meat or shellfish, dehydration, sudden weight loss, and some medications like thiazide diuretics. Long-term risks include kidney stones, tophi (lumpy crystal deposits under the skin), and links with high blood pressure, diabetes and chronic kidney disease.
You can’t blame one thing alone — genes, diet, medications and other health problems all add up. That’s why two people with similar diets can have very different gout risk.
Treating a flare right away
If you have an acute attack, start treatment fast. Good options are NSAIDs (naproxen or ibuprofen unless you have stomach or kidney problems), colchicine (a common early dose is 1.2 mg then 0.6 mg one hour later; older adults or those with kidney issues need lower doses), or a short course of oral corticosteroids. If a single joint is badly inflamed, a doctor may inject steroids directly into that joint.
Simple home steps help: rest and elevate the joint, apply ice for 15–20 minutes, and keep hydrated. Avoid alcohol and sugary drinks during a flare. If pain or swelling doesn’t improve in 48–72 hours, see a doctor — untreated flares can last days to weeks.
If your doctor suspects gout, they may remove fluid from the joint and look for crystals under a microscope. They’ll also check your serum uric acid level and screen for related health issues like kidney disease and high blood pressure.
Long-term control aims to lower uric acid so crystals dissolve and attacks stop. Urate‑lowering therapy (ULT) like allopurinol or febuxostat is advised when you have frequent flares (often two or more a year), tophi, or kidney stones from uric acid. Doctors usually start low and slowly increase the dose to reach a target uric acid — commonly under 6 mg/dL, and lower if you have tophi.
Practical prevention tips: lose weight gradually if you’re overweight, cut back on beer and sugary drinks, limit organ meats and shellfish, drink more water, and review medications with your doctor (some drugs raise uric acid). If you start ULT, your clinician may give anti-inflammatory cover for the first months because starting treatment can trigger flares as crystals shift.
Gout is manageable. With quick flare care and steady uric acid control, many people stop having attacks and keep joints working normally. Talk with your doctor about the right plan for you — simple changes plus the right medicine usually do the trick.