Herpes Zoster Hormones
When working with herpes zoster hormones, the hormonal factors that modulate the shingles virus and its symptoms. Also known as shingles hormone interactions, it bridges virology, endocrinology, and immunology to explain why some people get severe outbreaks while others barely notice a rash. Relatedly, Herpes Zoster, a reactivation of the varicella‑zoster virus that causes chickenpox and later shingles relies heavily on the Immune System, the body’s defense network of cells and chemicals that keep latent viruses in check. Hormonal shifts—especially in cortisol and estrogen—can tip that balance, making the virus flare up.
Key Hormonal Factors in Shingles
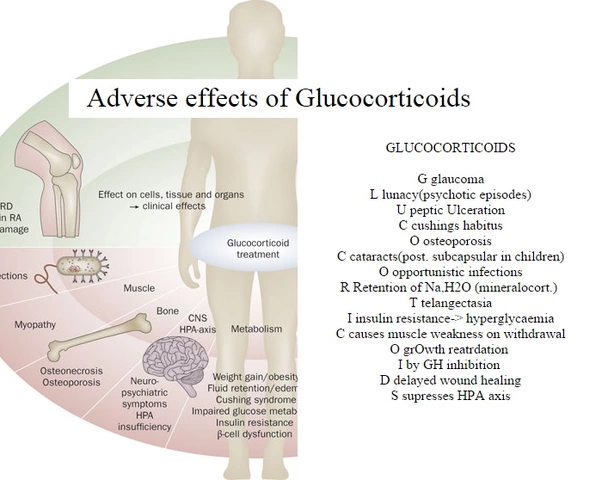
One of the most studied hormones is Cortisol, the primary stress hormone that suppresses inflammation and immune activity. High cortisol levels, whether from chronic stress or prolonged steroid use, dampen T‑cell function, the very cells that patrol for dormant viruses. This explains why patients on long‑term corticosteroids often see more aggressive shingles outbreaks. Another player is Estrogen, a sex hormone that can boost immune surveillance in women. Post‑menopausal drops in estrogen may reduce that protection, which is why older women sometimes report tougher shingles cases. Thyroid hormones also matter; hypothyroidism slows metabolism and can blunt the immune response, while hyperthyroidism may increase inflammation, each shaping the rash’s severity and pain.
Beyond individual hormones, the timing of vaccination interacts with hormonal status. The Shingles Vaccine, an approved immunization that raises virus‑specific antibodies works best when the immune system isn’t under hormonal suppression. Studies show that patients receiving the vaccine while on low‑dose steroids still develop protective antibodies, but the response is weaker than in hormone‑balanced individuals. This insight pushes clinicians to schedule vaccination before starting high‑dose steroid courses whenever possible.
Medication tolerance also ties into the hormone story. Drugs like betamethasone, a potent topical steroid, can thin skin and alter local cortisol levels, indirectly influencing how the shingles rash heals. Meanwhile, antiviral agents such as acyclovir work independently of hormones, but their efficacy can be compromised if the immune system is heavily suppressed. Understanding these overlaps helps doctors pick the right combo: a short steroid burst for inflammation control, followed quickly by antivirals to curb viral replication, all while monitoring hormone panels.
Putting it all together, the interplay of hormones, immune function, and medical interventions creates a complex web that determines how shingles shows up and resolves. Below you’ll find articles that dive into medication tolerance, heat safety for diuretic users, hormone‑linked fatigue, and more—each shedding light on pieces of this puzzle. Whether you’re looking for practical tips on managing side effects or deeper insight into how cortisol shapes skin health, the posts ahead give you actionable information to navigate herpes zoster hormones with confidence.