Lipid-Lowering Therapy: What It Is, How It Works, and What You Need to Know
When your blood fats—cholesterol and triglycerides—run too high, your risk for heart attack and stroke goes up. That’s where lipid-lowering therapy, a treatment approach designed to reduce harmful fats in the bloodstream. Also known as cholesterol-lowering treatment, it’s not just about popping a pill. It’s about managing long-term risk with proven medications, lifestyle changes, and sometimes a mix of both. This isn’t a one-size-fits-all fix. Some people see big drops with just a statin. Others need something stronger—or a combo—because their body doesn’t respond the same way.
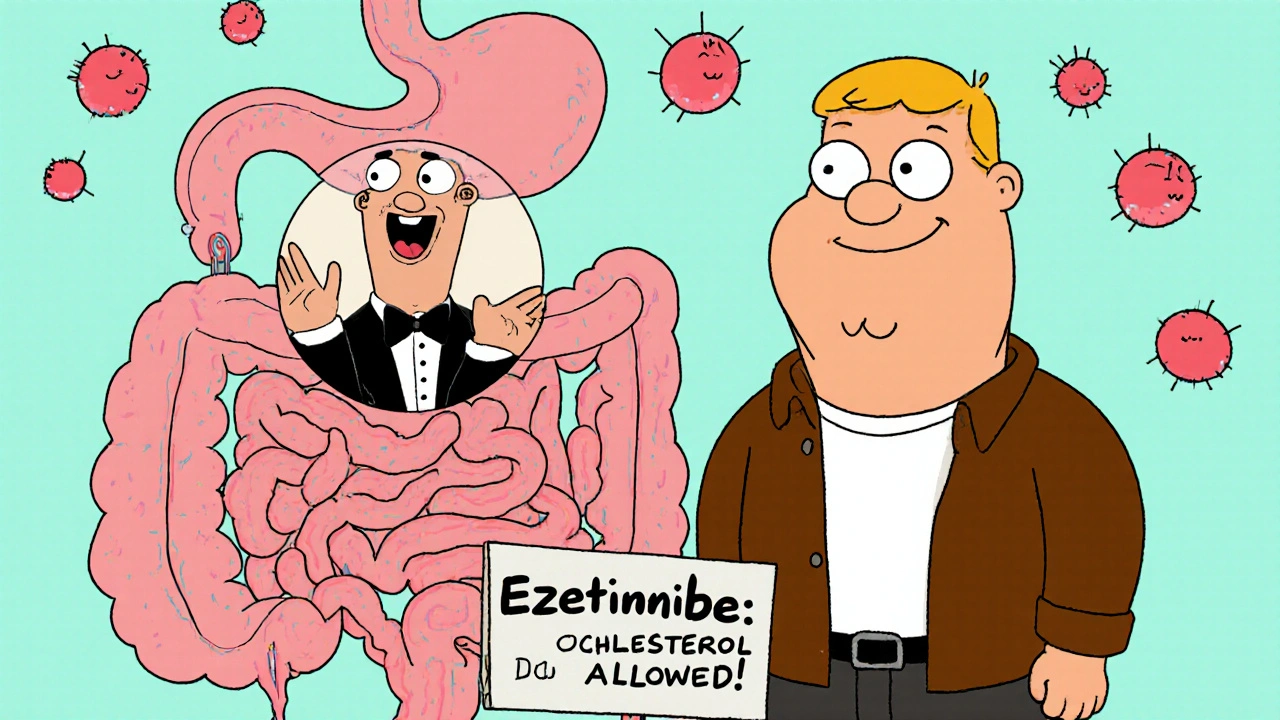
Two of the most common tools in this therapy are statins, a class of drugs that block cholesterol production in the liver. Also known as HMG-CoA reductase inhibitors, they’re the first line for most patients. Then there’s ezetimibe, a drug that stops the gut from absorbing cholesterol from food. Often paired with statins, it’s a go-to when statins alone aren’t enough—or when side effects like muscle pain make statins hard to tolerate. These aren’t magic bullets. They work best when you’re also eating better, moving more, and keeping weight in check. But for many, they’re the difference between managing risk and facing serious complications.
Not everyone needs medication right away. But if your numbers stay high despite diet and exercise, your doctor might suggest lipid-lowering therapy. And it’s not just about LDL—the "bad" cholesterol. Triglycerides matter too, especially if you’re diabetic or have metabolic syndrome. Some therapies target both. You might also hear about PCSK9 inhibitors or bile acid binders—those are for tougher cases, usually after other options fail.
Side effects? They happen. Muscle soreness with statins. Stomach upset with ezetimibe. But many of these fade over time, as your body adjusts. That’s why sticking with the plan matters. A lot of people quit because they feel fine after a few weeks—not realizing the real benefit is what’s not happening: no heart attack, no stroke, no emergency room visit.
The posts below cover real-world experiences with these treatments. You’ll find details on how ezetimibe affects digestion, why some side effects disappear after a few weeks, and how people manage cholesterol without always relying on statins. There’s also info on how other meds—like those for thyroid or diabetes—can interact with lipid therapy. Whether you’re just starting out or have been on treatment for years, you’ll find practical tips and clear comparisons to help you understand what’s working—and what’s not.