Off-Target Effects: What They Are and How They Impact Your Medications
When you take a medication, it’s meant to hit one specific target in your body—like blocking a receptor that causes pain or lowering cholesterol by inhibiting an enzyme. But sometimes, drugs don’t stick to the plan. They accidentally interact with other parts of your system, causing off-target effects, unintended biological responses caused by a drug acting on non-target molecules. Also known as off-target interactions, these are one of the main reasons why even well-designed drugs can cause unexpected side effects. This isn’t a flaw in you—it’s a flaw in the drug’s precision. Think of it like using a hammer to hang a picture but accidentally hitting your thumb instead. The hammer works fine for the job, but it’s not smart enough to avoid the thumb.
These effects show up in all kinds of ways: a blood pressure drug that makes you dizzy because it also affects your brain’s balance centers, or an antibiotic that triggers a yeast infection because it wipes out good bacteria along with the bad ones. The adverse drug reactions, harmful and unintended responses to medications at normal doses linked to off-target effects are why doctors track your symptoms closely when you start a new pill. It’s not just about allergies—it’s about the drug’s hidden fingerprints on your body. pharmacovigilance, the science of detecting, assessing, and preventing drug side effects exists because these reactions can be serious, even deadly. And while we can’t always stop them, we can spot them early using tools like dechallenge and rechallenge, clinical tests where stopping and restarting a drug confirms if it caused a side effect. If your rash disappears after you stop the pill and comes back when you restart it? That’s a clear signal the drug is the culprit, not something else.
What’s more, off-target effects aren’t random. They’re often tied to how drugs are tested. Generic drugs must match brand-name drugs in bioavailability, but small differences in how they’re made—called batch variability, differences between production lots that can alter drug behavior—can shift how the drug behaves in your body. One batch might hit its target cleanly; the next might drift slightly and trigger an off-target reaction. That’s why some people report different side effects with generics, even when they’re labeled the same. And while the FDA approves these drugs based on averages, your body doesn’t care about averages—it reacts to what’s in your pill today.
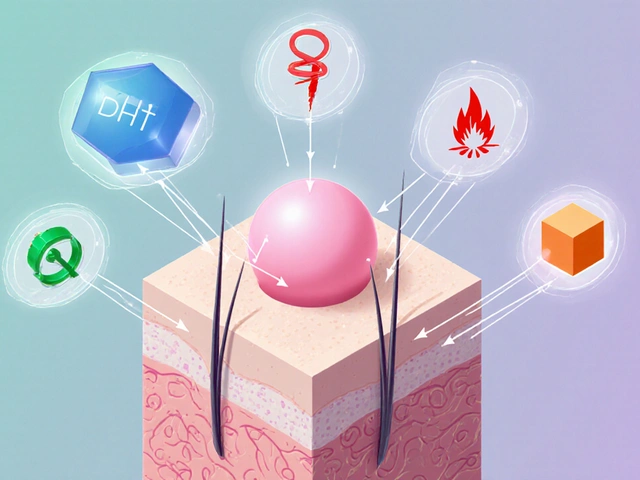
What you’ll find in the posts below isn’t theory. It’s real cases: how a common antihistamine triggered delirium in an older adult, why SGLT2 inhibitors raise yeast infection risk, how psychiatric drugs can clash dangerously, and how flavoring kids’ meds cuts side effects by making them easier to take. These aren’t isolated incidents—they’re all connected by the same hidden thread: drugs doing more than they were meant to. You don’t need a chemistry degree to protect yourself. You just need to know what to watch for, when to ask questions, and how to spot the signs before they become a problem.