Pheochromocytoma: Symptoms, Diagnosis, and Treatment Insights
When your body produces too much pheochromocytoma, a rare, usually noncancerous tumor that grows on the adrenal glands and overproduces stress hormones. Also known as adrenal chromaffin cell tumor, it triggers sudden, intense surges of adrenaline and noradrenaline—leading to headaches, sweating, heart palpitations, and dangerously high blood pressure. This isn’t just anxiety or stress. It’s a physical condition that mimics panic attacks but can cause heart damage, stroke, or even sudden death if ignored.
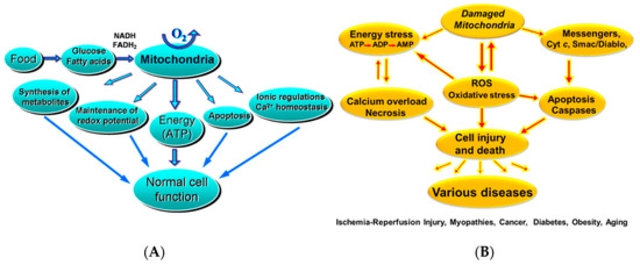
Pheochromocytoma is closely tied to catecholamines, the group of hormones—including adrenaline—that control heart rate, blood pressure, and metabolism. When the tumor is active, these chemicals flood your system without warning. That’s why symptoms often come in waves: a racing heart, dizziness, nausea, or a feeling of impending doom—all while your blood pressure spikes to levels you’ve never seen before. Many people are misdiagnosed with anxiety or hypertension for years before testing reveals the real culprit.
Diagnosis isn’t simple. Doctors look for elevated levels of metanephrines in urine or blood—markers that show your body is overproducing these hormones. Imaging like CT or MRI scans then locate the tumor. In some cases, it’s found by accident during tests for other issues. But if you’ve had unexplained spikes in blood pressure, especially with family history of similar tumors, testing is critical. paraganglioma, a related tumor that can form outside the adrenal glands, often in the neck or abdomen shares the same hormone patterns and requires the same careful approach.
Treatment usually means surgery to remove the tumor, but it’s not as simple as just cutting it out. Before surgery, you need months of medication to block the effects of excess hormones—drugs like alpha-blockers and beta-blockers stabilize your blood pressure and protect your heart. Skipping this step can be deadly during surgery. After removal, most people recover fully, but regular follow-ups are needed because these tumors can come back—or appear in other spots.
What you’ll find in the posts below isn’t a textbook on endocrinology. It’s real-world guidance from people who’ve dealt with similar conditions: how medications like beta-blockers affect daily life, how to track symptoms that doctors might miss, what tests actually matter, and how to talk to your provider when something feels off. You won’t find fluff here—just clear, practical info that helps you ask the right questions and understand what’s really going on inside your body.