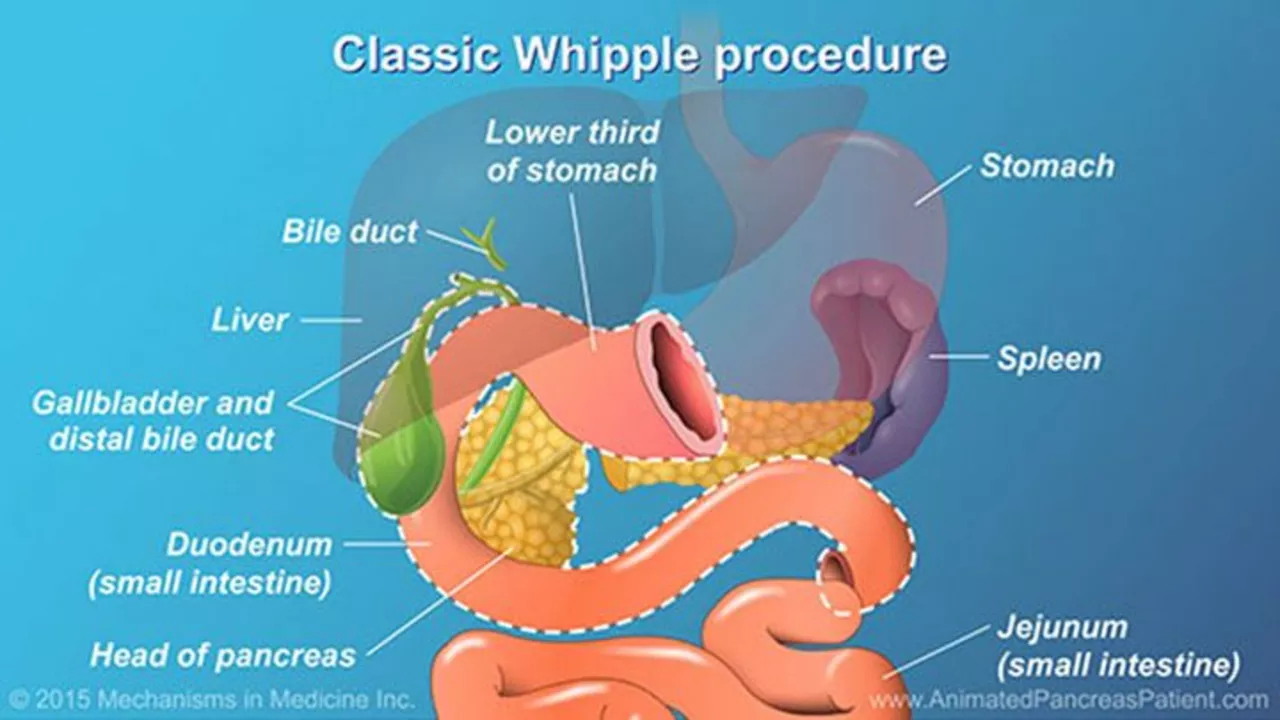
Post-Whipple Surgery Recovery: What to Expect and How to Recover
Undergoing a Whipple (pancreaticoduodenectomy) changes how your digestion works. Recovery is slow but manageable when you know what to expect. This guide gives clear, practical steps for the hospital stay and the weeks after so you can focus on healing without guessing what’s normal.
What to expect in hospital
Right after surgery you'll have drains, IV fluids, and often a tube in your nose. Expect 5–10 days in the hospital for most people, sometimes longer if complications pop up. Nurses will watch your drainage volume and color, check your blood sugars, and make sure your bowels start moving again.
Pain will be managed with a combination of IV meds, oral opioids, or nerve blocks. Tell staff if pain stops you from coughing, moving, or breathing deeply—those actions lower lung and clot risks. Start gentle walking the day after surgery. Even short walks to the door help reduce stiffness and pneumonia risk.
Practical tips for the weeks after
At home your energy will be low for several weeks. Plan help for cooking and chores. Eat small, frequent meals—think 5–6 mini-meals daily—because your stomach and pancreas need time to adjust. Focus on soft, protein-rich foods: scrambled eggs, yogurt, cottage cheese, well-cooked fish, and blended soups. Avoid heavy, greasy meals at first.
Pancreatic enzyme replacement is common if you have trouble digesting fats. Your surgeon or GI team will tell you the dose and when to take enzymes (usually with meals). If you notice oily stools, bloating, or weight loss, mention it—dosing often needs adjustment.
Blood sugar can become unstable after a Whipple because part of the pancreas may be removed. Monitor glucose as advised. If you already had diabetes, your meds may change. If not, watch for new symptoms: excessive thirst, frequent urination, or unexplained fatigue. Contact your team if levels run high or low.
Wound care is usually straightforward: keep the incision clean and dry, watch for redness, drainage, or fever. Light activity is okay, but avoid heavy lifting (no more than 5–10 pounds) for 6–8 weeks or until cleared. Driving is off-limits while on narcotics or until you can react normally.
Common issues after Whipple include delayed gastric emptying (feeling full, nausea), infections, or leaks from reconnections. These show up as increasing belly pain, fever, persistent vomiting, or sudden changes in drain output. Call your surgeon if these happen.
Follow-up appointments are crucial. You’ll need wound checks, nutritional review, and scans or blood tests depending on the reason for surgery. Bring a list of symptoms and any medications you can’t tolerate—this helps the team fine-tune your care quickly.
Small, steady progress matters more than pushing too hard. Rest, eat often, stay hydrated, walk a little each day, and report any worrying signs early. With patience and the right support, most people regain strength and adapt to life after a Whipple.