Serotonin Syndrome: Causes, Signs, and Medications That Trigger It
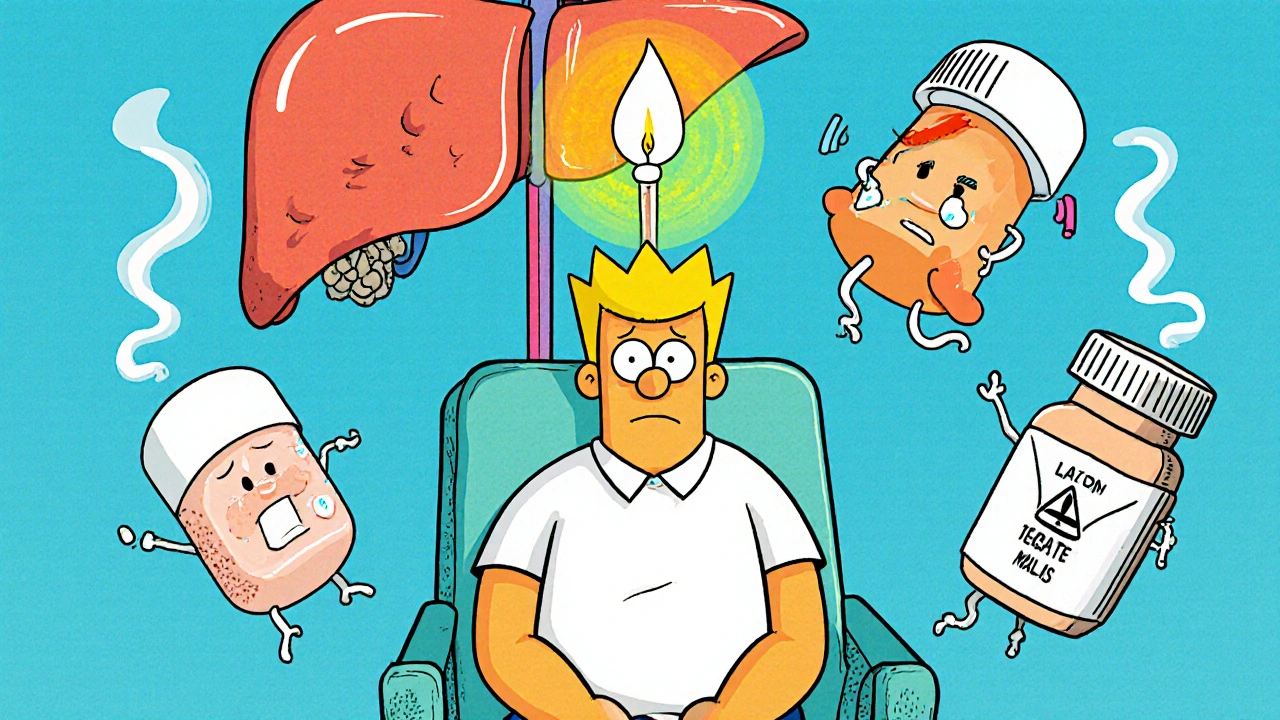
When your body gets too much serotonin, a natural chemical that helps regulate mood, sleep, and digestion. Also known as serotonin toxicity, it’s not just a side effect—it’s a medical emergency that can escalate fast. This happens when medications pile up and push serotonin levels past what your brain can handle. It’s not rare, and it’s often missed because symptoms look like the flu, anxiety, or heat exhaustion.
Common culprits include antidepressants, especially SSRIs and SNRIs like sertraline, fluoxetine, and venlafaxine, paired with other drugs like triptans, used for migraines, or even over-the-counter cough syrups with dextromethorphan. Even adding a new supplement like St. John’s wort or tryptophan can tip the scale. The risk spikes when people take multiple drugs at once—something caregivers often miss when managing polypharmacy in older adults.
You don’t need to be on all these drugs to get serotonin syndrome. Sometimes, just increasing the dose of one medication is enough. Symptoms start within hours: shivering, diarrhea, fast heartbeat, high blood pressure, muscle stiffness, or confusion. In severe cases, fever, seizures, or loss of consciousness can happen. If you’re on antidepressants and suddenly feel worse after a new prescription or dose change, don’t wait—get help. Many of the posts here cover how to track drug interactions, spot hidden risks in medication lists, and understand why some side effects aren’t just "normal"—they’re warning signs.
What you’ll find below are real-world guides on how medications interact, how to monitor for dangerous reactions, and what to ask your doctor before adding anything new. From dechallenge tests that prove a drug caused a reaction, to how antipsychotics and other psychiatric meds can add to the risk, these posts give you the tools to spot trouble before it’s too late. This isn’t theory—it’s about keeping yourself or someone you care for safe while taking necessary medicines.