SGLT2 Inhibitors: How These Diabetes Drugs Work and What You Need to Know
When you hear SGLT2 inhibitors, a class of oral diabetes medications that lower blood sugar by making the kidneys remove excess glucose through urine. Also known as gliflozins, these drugs don’t just manage blood sugar—they’ve been shown to reduce heart failure hospitalizations and slow kidney damage in people with type 2 diabetes. Unlike older diabetes pills that force your body to make more insulin or make cells more sensitive to it, SGLT2 inhibitors work differently: they block a protein in your kidneys that normally reabsorbs sugar back into your blood. Instead, that sugar leaves your body through urine. It’s like turning your kidneys into a natural sugar filter.
This mechanism means they work even when insulin levels are low, which is why they’re often used alongside metformin or other meds. Three main drugs fall under this category: empagliflozin, a once-daily pill shown in large studies to cut heart-related deaths in high-risk patients, dapagliflozin, linked to improved kidney outcomes and weight loss, and canagliflozin, the first in the class, known for reducing A1C and helping with modest weight reduction. These aren’t just sugar-lowering tools—they’ve changed how doctors think about treating diabetes, especially when heart or kidney health is also a concern.
But they’re not without trade-offs. Because they make you pee out more sugar, you might notice more frequent bathroom trips, especially at first. There’s also a small risk of genital yeast infections, especially in women, and a rare but serious condition called diabetic ketoacidosis—even when blood sugar isn’t very high. Dehydration is another concern, so drinking enough water matters. These drugs also tend to cause a little weight loss, which many people welcome, but they can lower blood pressure, so dizziness when standing up can happen. If you’re on a diuretic or have kidney issues, your doctor will need to monitor you closely.
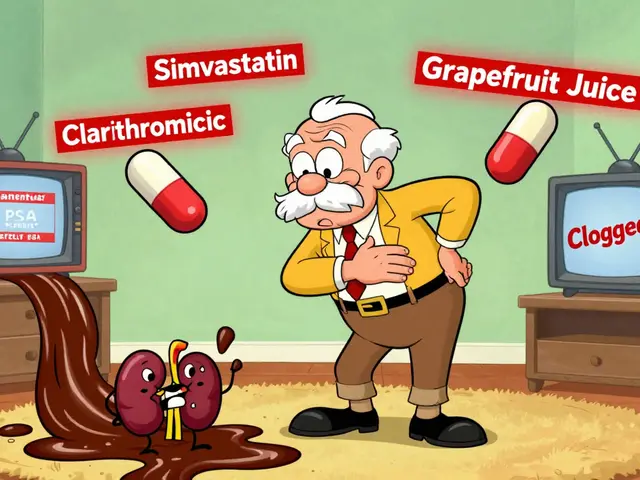
What you’ll find in the posts below is a practical look at how these drugs fit into real-life care. You’ll see how they connect to other treatments like statins and ezetimibe for heart health, how they relate to metabolic risks seen with antipsychotics, and how medication lists and tolerance patterns play out when you’re taking multiple drugs long-term. These aren’t just clinical facts—they’re lived experiences. Whether you’re managing diabetes yourself, helping a loved one, or just trying to understand why your doctor picked this pill over another, the information here is meant to make sense of the bigger picture.