Understanding TIA vision problems: Causes, Symptoms, and What to Do
When dealing with TIA vision problems, temporary visual disturbances that occur during a transient ischemic attack. Also known as mini‑stroke eye symptoms, they signal a brief interruption of blood flow to the visual pathways. Transient Ischemic Attack is a short‑lived episode of neurological dysfunction, and stroke often follows if the warning signs are ignored. The visual system can react with visual field loss, double vision, or curtain‑like blind spots, each hinting at which part of the brain or eye is affected. Recognizing these signs early can cut the risk of a full‑blown stroke by up to 80%. [TIA vision problems] encompasses temporary loss of sight; [Transient Ischemic Attack] requires immediate medical evaluation; and [stroke] is increased by previous TIA episodes. These three entities create a clear cause‑effect chain that makes early detection vital.
Risk Factors, Diagnosis, and First‑Line Treatment
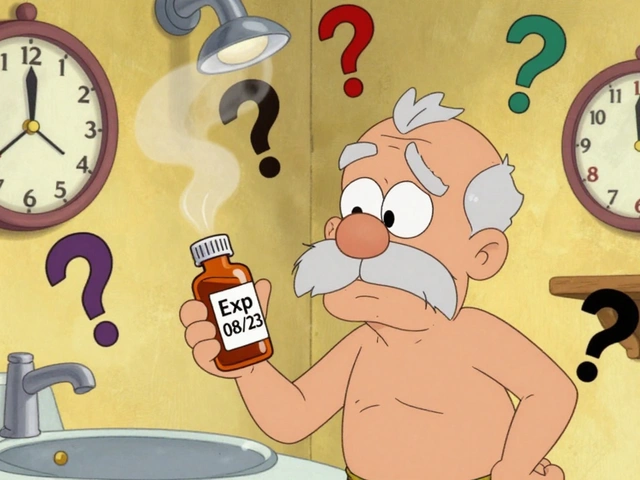
Vision problems during a TIA happen because the retina or the optic radiations receive less oxygen for a few minutes. Common risk factors—high blood pressure, diabetes, smoking, and atrial fibrillation—create the plaque buildups that can temporarily block arteries. Hypertension is the single most modifiable factor; lowering systolic pressure by 10 mmHg can halve the chance of a repeat event. The side of the visual loss often matches the side of the brain lesion: a right‑handed loss points to the left occipital lobe, while a left‑handed loss suggests right‑side involvement. Younger adults aren’t immune; about 20% of TIA cases involve people under 50, especially those with uneven cholesterol or family histories of clotting disorders. A fast‑track assessment is essential: a CT or MRI rules out bleeding, carotid ultrasound checks for narrowing, and blood panels reveal clotting abnormalities. Antiplatelet drugs such as aspirin or clopidogrel lower the chance of a repeat event, while statins stabilize plaque. If carotid narrowing exceeds 70%, a surgeon may recommend endarterectomy, which can reduce future stroke risk by more than 70%. Lifestyle tweaks—cutting salt, exercising, quitting smoking—address the root causes and complement medication. Patients often ask how long the visual symptoms last. Most episodes resolve within 10‑30 minutes, but some linger up to a few hours, leaving a temporary “after‑image” or mild haze. Even after the vision clears, the brain undergoes a stress response that can affect memory and balance for a day or two. Follow‑up care should include a neurologist visit within 24‑48 hours and a comprehensive eye exam to document any residual field deficits. Early rehabilitation, like vision therapy, can help retrain the brain’s visual pathways and improve quality of life. In everyday terms, think of TIA vision problems as an early fire alarm for your brain’s blood supply. Ignoring the alarm invites a bigger blaze—stroke—that can cause permanent blindness or paralysis. By spotting the warning, getting the right tests, and starting treatment fast, you turn a fleeting visual glitch into a lifesaver. Below you’ll find a curated set of articles that break down the drugs, risk‑factor management, and practical tips you need to handle TIA‑related visual issues. From medication tolerability to heat‑safety for those on diuretics, the collection gives you a full picture of how to stay ahead of the next episode.