Vertigo: Why the Room Spins and What to Do Now
Feeling the room spin when you move your head? That spinning is vertigo — a false sense that you or the world around you is moving. It’s not the same as lightheadedness. Vertigo often brings nausea, sweating, and trouble walking. It can be short and harmless or a sign of something serious. Knowing the likely causes helps you act fast.
Causes and what to watch for
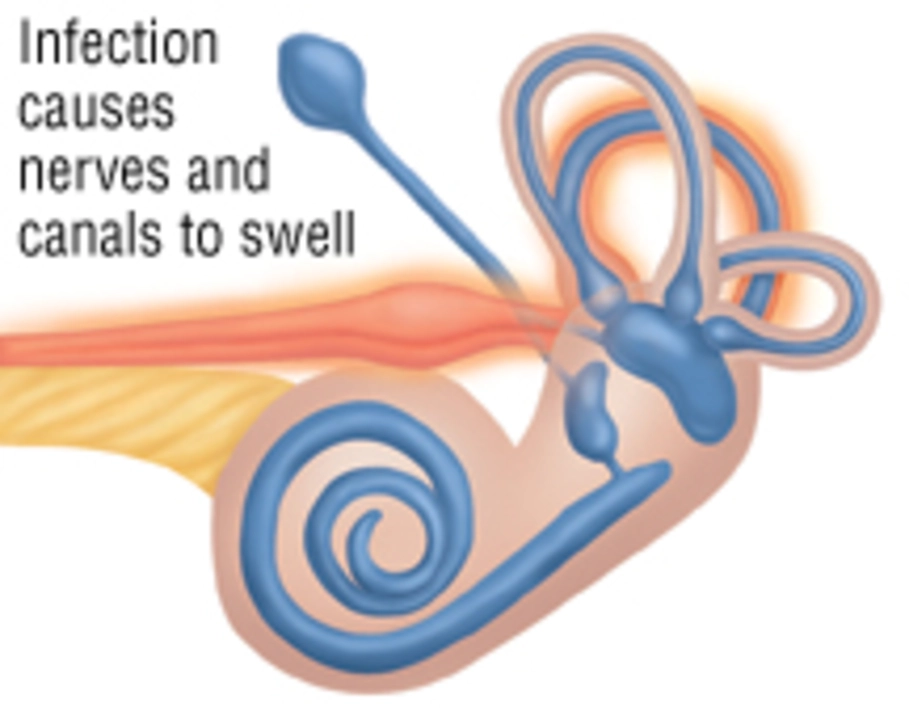
The most common cause is benign paroxysmal positional vertigo (BPPV). Tiny calcium crystals in the inner ear shift and trigger short, strong spinning when you tilt your head. Vestibular neuritis is usually viral and causes longer, constant vertigo with imbalance. Meniere’s disease pairs vertigo with hearing loss, ear fullness, and sometimes tinnitus. Migrainous vertigo can occur with or without a headache. Medications, low blood pressure, and head injury also cause vertigo. Rarely, sudden severe vertigo with weakness, slurred speech, or vision trouble points to a stroke.
Doctors use quick bedside tests to spot BPPV, like the Dix-Hallpike, and may order hearing tests or an MRI if they suspect something more serious. Write down when spells happen, what you were doing, how long they last, and any hearing or vision changes. That info speeds diagnosis.
Quick steps and treatments you can try
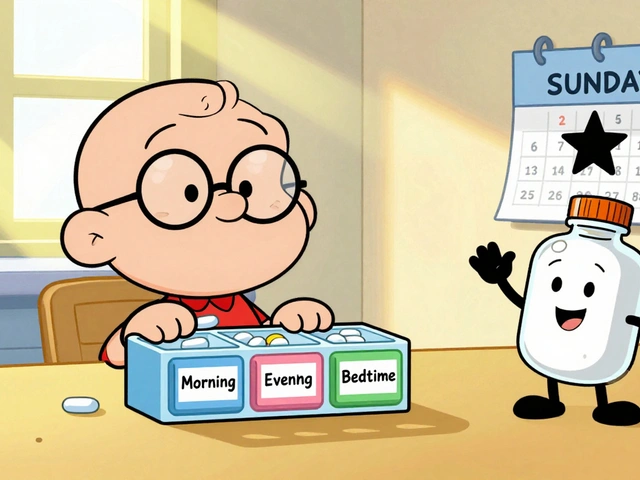
If a spell starts, sit or lie down right away. Keep your eyes closed and breathe slowly. Avoid driving or climbing stairs until you feel steady. For BPPV the Epley maneuver can stop spells in most people after a few repetitions; ask a clinician or watch a medical source video to learn the steps. Over-the-counter meclizine or prescription vestibular suppressants can ease symptoms short-term, and anti-nausea meds help with vomiting.
Vestibular rehabilitation therapy (VRT) is physical therapy for balance. It teaches exercises and head movements that retrain your brain and reduce long-term dizziness. For Meniere’s, doctors may suggest a low-salt diet and diuretics. If vertigo comes from migraine, treating the migraine prevents many attacks.
See urgent care if vertigo comes on suddenly with weakness, numbness, trouble speaking, or double vision. Make a routine appointment if spells are frequent or getting worse. A simple diary and a quick exam usually point the clinician to the right fix.
Small changes help: sleep slightly elevated, rise slowly from bed, cut alcohol and caffeine, and use railings. If spells affect work or driving, tell your employer and avoid risky tasks until you have a clear treatment plan.
If you want help deciding next steps, start with your primary doctor or an ENT. Vestibular physical therapists are often the most useful follow-up. With the right diagnosis, vertigo is often controllable, and you can get back to normal activities.
Many people see big improvement within days to weeks with proper treatment. BPPV often responds quickly to repositioning maneuvers, while vestibular neuritis may need weeks of rehab. Chronic dizziness can improve over months with consistent exercises. If treatments fail, ask about imaging or referral to a balance clinic — persistence usually pays off. Get help early and don’t ignore symptoms.