Why Talking to Your Doctor About Your Medications Matters More Than You Think
Half of all people with chronic conditions don’t take their medicines as prescribed. That’s not laziness. It’s not forgetfulness alone. It’s often because they don’t feel heard, understood, or supported when they talk to their doctor. If you’ve ever skipped a pill because the side effects scared you, or stopped taking something because it was too expensive, or just didn’t know why you were taking it in the first place-you’re not alone. And your doctor needs to know.
The truth is, your doctor can’t help you if they don’t know what’s really going on. A 2021 study found that when doctors ask open-ended, non-judgmental questions like, “Many people have trouble taking their meds on time. Does that happen to you?”, patients are 37% more likely to be honest. That one shift in wording changes everything. It turns a confrontation into a conversation.
What Happens When You Don’t Talk About It
Skipping doses, stopping early, or mixing pills without telling your doctor doesn’t just make your condition worse-it puts you at risk for hospital visits, emergency care, and even death. In the U.S., medication errors linked to poor communication cause about 7,000 deaths each year, according to the FDA. For people with high blood pressure, diabetes, or heart disease, missing just a few doses can lead to a stroke, heart attack, or kidney failure.
And the costs go beyond health. Non-adherence adds $300 billion to the U.S. healthcare system every year. Hospitals pay more to readmit patients who didn’t take their meds-30-day readmission rates jump from 14.8% for those who follow their plan to 22.4% for those who don’t. That’s why clinics now track adherence as part of their performance. It’s not just about your health. It’s about the system trying to catch up.
What Doctors Are Trained to Do (But Often Don’t)
Doctors aren’t ignoring you. Most want to help. But many weren’t taught how to have these conversations. A 2022 survey found that 82% of physicians say they don’t have enough time to dig into why patients aren’t taking their meds. But here’s the fix: it doesn’t take long. Just two or three extra minutes per visit can make a huge difference.
Training programs now teach doctors five key steps:
- Ask open-ended questions. Instead of “Are you taking your pills?” try “What’s your routine been like with your medications this past week?”
- Listen without interrupting. If you say you’re having side effects, don’t let them cut you off. Let them hear you.
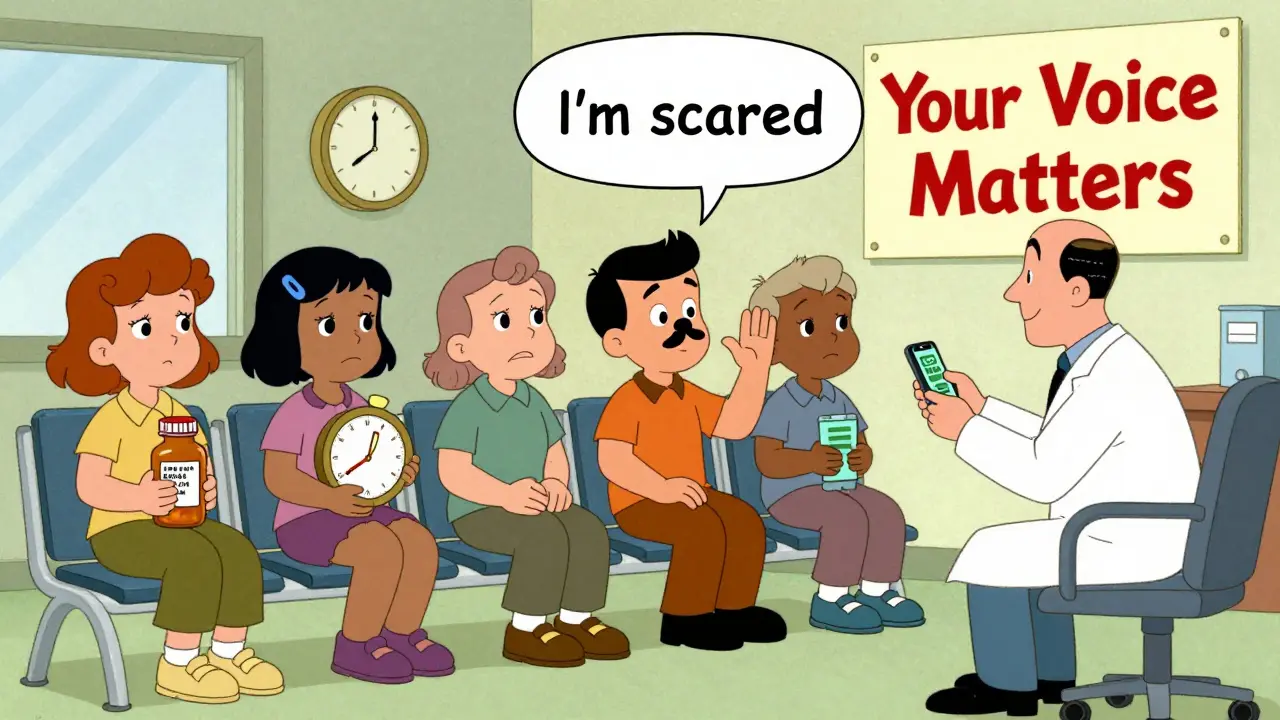
- Validate your feelings. If you say, “I’m scared of the side effects,” they should respond with, “That’s a real concern. Many people feel the same way.”
- Explain in plain language. No jargon. No “hypertension.” Say “high blood pressure.” If they use a word you don’t know, ask them to explain it.
- Write it down. Ask them to write your meds, doses, and times on a piece of paper. Keep it. Show it to your pharmacist.
This isn’t theory. The “teach-back” method-where you repeat back what you heard in your own words-boosts adherence by 17%. That’s the same as adding a new drug to your regimen, but without the cost or side effects.
How to Prepare Before Your Appointment
You don’t have to wait for your doctor to ask. Come ready to talk. Here’s what to bring:
- A list of every medication you take-prescription, over-the-counter, vitamins, supplements. Don’t leave anything out.
- Notes on when you miss doses and why. Was it because you forgot? Were the pills too big? Did they make you dizzy? Did they cost too much?
- Questions written down. Examples: “Can this be taken with food?” “Is there a cheaper version?” “What happens if I skip one day?”
If you’re nervous, practice saying it out loud. Try: “I’ve been having trouble taking my blood pressure pill because it makes me tired after lunch. I’m not sure if I should keep taking it.” That’s honest. That’s helpful. That’s what your doctor needs to hear.
What to Do If Your Doctor Doesn’t Listen
Not all doctors are trained in communication. If you feel dismissed, judged, or rushed, you have options. You’re not stuck.
First, try asking directly: “I want to make sure I’m doing this right. Can we talk about what’s making it hard for me to take my meds?” If they still brush you off, ask for a nurse, pharmacist, or care coordinator. Many clinics now have medication adherence specialists who spend 20-30 minutes with patients one-on-one.
If you’re still not heard, it’s okay to switch doctors. Your health isn’t negotiable. A 2023 study found that patients who switched to providers who used patient-centered communication saw a 23% improvement in adherence within six months. That’s not luck. That’s better care.
Real Stories: What Worked for Real People
One patient in Birmingham stopped taking her heart medication after her doctor scolded her for missing one dose. She felt ashamed. She lied for months. Then her body started rejecting her transplant. She only told the truth when a new doctor asked, “What’s the hardest part about taking your pills?” That question saved her life.
Another man, 71, stopped taking his diabetes pills because he didn’t understand why he needed them. He thought the sugar in his blood would “just go away.” His pharmacist sat down with him for 15 minutes, drew a picture of his pancreas, and showed him how the medicine worked. He started taking them. His A1C dropped from 9.8 to 6.4 in three months.
These aren’t rare cases. They’re common. And they all started with one simple thing: someone asked the right question.
Technology Can Help-But Only If You’re Ready
There are apps, pill boxes with alarms, and smart bottles that text your doctor if you miss a dose. But tech won’t fix a bad conversation. A 2023 report found that AI chatbots and digital reminders improve adherence by only 12%-unless they’re paired with human support. The real wins come when a person listens, understands, and adjusts your plan based on your life.
If you’re over 65, or don’t use smartphones often, don’t feel pressured to use tech. Paper lists, pill organizers, and calendar reminders still work. The goal isn’t to be high-tech. It’s to be consistent.
What’s Changing in 2026
Starting in 2024, the American Medical Association made communication skills part of the evaluation for doctors in value-based care programs. That means if your doctor doesn’t ask about your meds, they could lose money. That’s a big shift. It’s no longer optional. It’s part of the job.
Hospitals in the U.S. are now required to check medication adherence before discharge. If you’re going home after surgery or a hospital stay, they must ask you: “Do you understand what you’re taking and why?” If you say no, they have to fix it before you leave.
And it’s working. Systems that use structured communication have a 92% success rate keeping these practices going long-term. That’s higher than any app, device, or reminder system.
Your Role in This
You’re not a patient who’s supposed to follow orders. You’re a partner in your care. You know your body better than anyone. If something feels off, say it. If you can’t afford your pills, say it. If you’re scared, say it. Your doctor can’t help you if they don’t know the truth.
Medication adherence isn’t about being perfect. It’s about being honest. It’s about showing up-not just for your pills, but for your own health. And the best tool you have isn’t a pillbox or an app. It’s your voice.
Why do doctors ask if I’m taking my meds, even if I say I am?
Doctors ask because studies show up to half of patients say they take their meds when they don’t. It’s not about distrust-it’s about accuracy. Many people skip doses without realizing it’s a problem. Others stop because of side effects but are too embarrassed to say so. By asking in a calm, non-judgmental way, doctors can find the real reason and fix it.
What if I can’t afford my prescriptions?
Tell your doctor. They may be able to switch you to a generic version, connect you with a patient assistance program, or give you samples. Many drug companies offer free or low-cost meds for people who qualify. Pharmacists can also help-ask them during your refill. You’re not alone. One in five Americans struggle with medication costs. Your doctor’s job is to find a solution, not to judge your situation.
Can I stop taking a medication if I feel better?
Only if your doctor says so. Many medications-like blood pressure or cholesterol drugs-work even when you feel fine. Stopping them can cause your condition to come back harder than before. If you think you don’t need it anymore, talk to your doctor first. They can check your numbers and decide if it’s safe to adjust or stop.
What if I forget to take my pills often?
Forgetfulness is one of the most common reasons people miss doses. Try linking your meds to a daily habit-like brushing your teeth or eating breakfast. Use a pill organizer with days of the week. Set alarms on your phone. If you’re still struggling, ask your doctor about once-daily options or combination pills that reduce the number of doses you need.
Is it okay to ask my doctor to explain my meds again?
Absolutely. No doctor should make you feel silly for asking. If you don’t understand why you’re taking a medicine, how it works, or what side effects to watch for, you’re not ready to take it safely. Ask them to explain it like you’re a 12-year-old. If they can’t, ask for a pharmacist. You deserve to know what’s in your body.