Ketamine and Esketamine: Rapid-Acting Options for Treatment-Resistant Depression
If you’ve tried multiple antidepressants and still feel stuck in deep depression, you’re not alone. About 3 in 10 people with major depression don’t get relief from standard meds. For these cases, traditional pills can take weeks-sometimes months-to work. But what if relief could come in hours? That’s where ketamine and esketamine come in.
These aren’t your usual antidepressants. They’re fast-acting, powerful tools that can lift the fog of depression faster than anything else available today. But they’re not the same. One is given through an IV. The other is a nasal spray. One is FDA-approved for depression. The other isn’t-yet still widely used. And the differences matter a lot when you’re trying to decide what’s right for you.
How Ketamine and Esketamine Work
Both ketamine and esketamine target the brain differently than SSRIs or SNRIs. Instead of boosting serotonin or norepinephrine, they block NMDA receptors. This triggers a cascade of effects: new connections form between brain cells, inflammation drops, and the brain’s ability to adapt improves. Think of it like rebooting a frozen computer.
Ketamine is a racemic mix-meaning it contains both (R)- and (S)-enantiomers. Esketamine is just the (S)-part. That small chemical difference changes how the drug behaves in your body. Esketamine produces fewer dissociative side effects-less of that out-of-body feeling-but also seems to work more slowly.
A 2025 study from Mass General Brigham tracked 153 patients with treatment-resistant depression. Those getting IV ketamine saw a 49.22% drop in depression scores after their full course. Those on nasal esketamine saw a 39.55% drop. That’s not just a small gap-it’s a clinically meaningful difference.
Administration: IV vs. Nasal Spray
How you get the drug changes everything.
IV ketamine is given in a clinic over 40 minutes. A needle goes into your arm. You’re monitored closely. You might feel dizzy, floaty, or see colors. That’s normal. Most people feel better within hours. One treatment can be enough to shift your mood.
Esketamine (Spravato®) is a nasal spray. You sit in a doctor’s office, spray it up your nose, and wait. No needle. No IV. But you still need to stay for two hours after each dose. You can’t drive yourself home. The dose starts at 56 mg, then may go up to 84 mg twice a week during the first month.
The Mass General Brigham study found IV ketamine patients felt better after their first treatment. Esketamine patients didn’t see real improvement until their second. That’s critical if you’re in crisis.
Efficacy: Which One Works Faster and Better?
It’s not just about speed-it’s about depth of response.
Research published in the Journal of Clinical Psychiatry in September 2025 showed that IV ketamine produced stronger and faster symptom relief across all measures. Patients reported clearer thinking, less hopelessness, and reduced suicidal thoughts sooner.
A 2020 meta-analysis of 18 studies confirmed this pattern: IV ketamine consistently outperformed nasal esketamine in reducing depression scores from 24 hours to eight weeks after treatment.
Real-world data backs this up. On PatientsLikeMe, 63.2% of IV ketamine users said they felt significant relief within 24 hours. For esketamine users, that number was 51.7%. If you’re desperate for quick relief, the data points to IV ketamine.
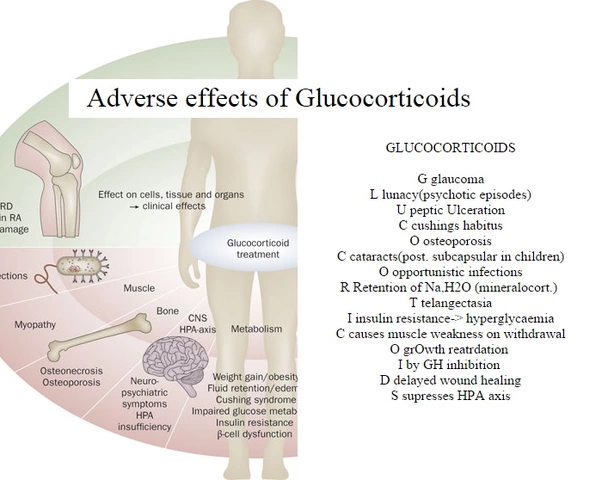
Safety and Side Effects
Both drugs can cause dissociation-feeling detached from your body or surroundings. But the intensity differs.
In the 2025 study, 42.3% of IV ketamine patients reported moderate to severe dissociation. For esketamine, it was 28.7%. That’s a 37% lower rate of severe effects with the nasal spray.
Esketamine also has a lower risk of abuse because it’s administered under strict supervision. IV ketamine, while effective, carries higher potential for misuse if not tightly controlled. Both are Schedule III controlled substances-meaning they have accepted medical use but can lead to dependence.
Long-term safety data is still limited. But so far, neither drug shows signs of brain damage or organ toxicity at therapeutic doses. The biggest concern? Repeated use without proper follow-up. Both require ongoing monitoring.
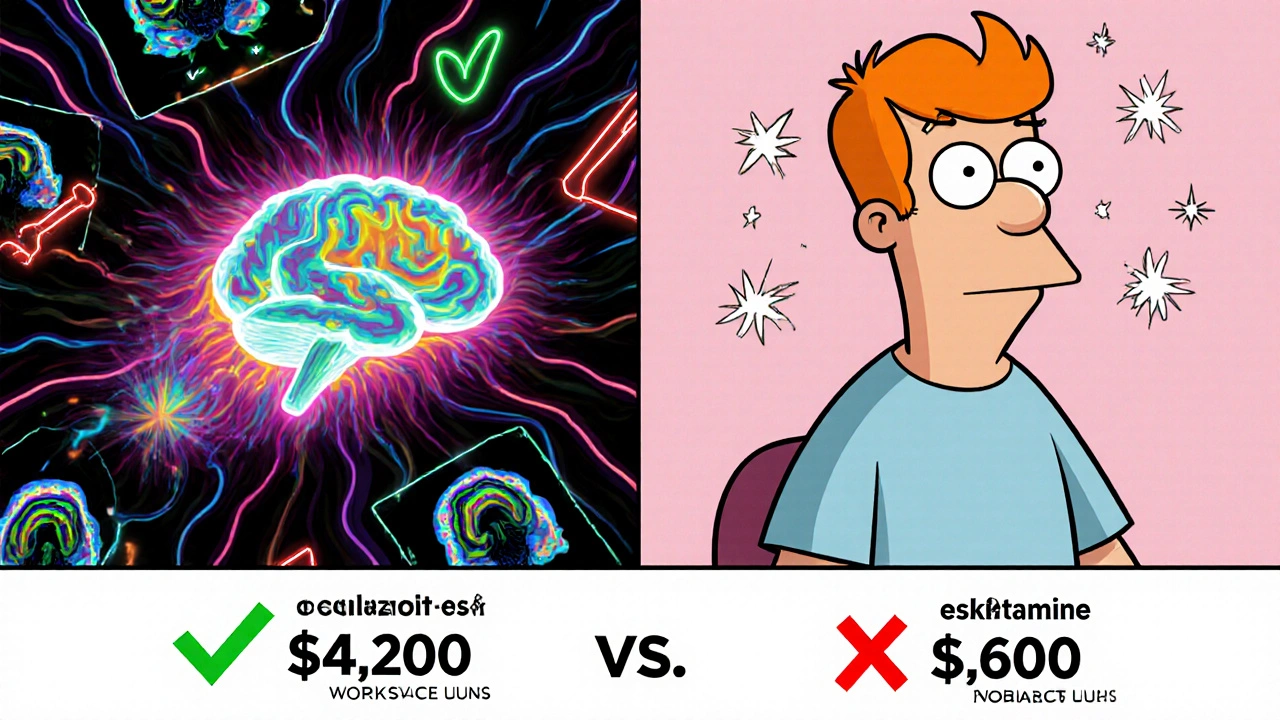
Cost and Insurance Coverage
Money matters. A full course of eight IV ketamine infusions costs between $4,200 and $5,600. A similar course of Spravato® runs $5,800 to $6,900.
But here’s the twist: insurance covers esketamine far more often. 67.4% of commercial plans cover Spravato®. Only 38.2% cover IV ketamine-even though it’s cheaper and often more effective.
Why? Because esketamine is branded, FDA-approved for depression, and comes with manufacturer support programs. IV ketamine is used off-label. Most insurers see it as experimental-even though it’s been used for depression for over 20 years.
A 2025 JAMA Psychiatry cost-effectiveness analysis found IV ketamine delivers better value: $14,327 per quality-adjusted life year (QALY) gained. Esketamine was $18,764 per QALY. In plain terms: IV ketamine gives you more health improvement for less money.
Who Gets Which Treatment?
There’s no one-size-fits-all answer. But experts have clear preferences based on patient needs.
Dr. John Krystal at Yale says IV ketamine is best for “life-threatening depression”-when someone is actively suicidal and needs immediate relief. The faster, stronger response matters.
Dr. Christine Denny at Columbia argues esketamine is better for long-term maintenance. Less intense side effects. Easier to fit into a routine. More convenient for outpatient care.
Here’s a simple guide:
- Choose IV ketamine if: You’re in acute crisis, need fast results, can’t wait weeks, and are okay with more intense side effects.
- Choose esketamine if: You prefer a non-invasive option, have milder symptoms, want to avoid IVs, and are planning long-term maintenance.
Both require an oral antidepressant to be taken alongside them. Neither is a standalone cure.
Access and Availability
Getting either treatment isn’t easy.
As of 2025, only 12.4% of U.S. counties have certified Spravato® centers. IV ketamine clinics are slightly more common-but still rare. The number of ketamine clinics jumped from 142 in 2020 to over 1,000 in 2025, but most are concentrated in big cities.
Most insurance plans require you to try at least two antidepressants first. You need a diagnosis of treatment-resistant depression. Clinics often require a referral from a psychiatrist.
And you can’t just walk in. Both require supervised administration. You can’t take ketamine home. You can’t self-administer esketamine. Both need a medical setting with trained staff and emergency equipment.
What’s Next?
The field is moving fast.
In September 2025, the FDA accepted a new application for a higher-dose Spravato® (112 mg). That could mean faster results with fewer doses.
Researchers are also testing intramuscular ketamine-injections in the muscle. That could offer a middle ground: faster than nasal, less invasive than IV.
And there’s new hope in brain imaging. A November 2025 study in Nature Mental Health found that increased gamma wave activity in the frontoparietal region of the brain predicts who will respond to ketamine. In the future, a simple EEG might tell your doctor if this treatment will work for you.
Final Thoughts
Ketamine and esketamine aren’t magic pills. But for people who’ve hit dead ends with traditional antidepressants, they’re the most promising breakthrough in decades.
IV ketamine works faster and stronger. It’s cheaper. But it’s harder to access, more intense, and often not covered by insurance.
Esketamine is easier to tolerate. Easier to get approved for insurance. But it’s pricier and slower. It’s better for stability than crisis.
The best choice depends on your situation: how bad your depression is, how fast you need relief, what you can afford, and what kind of experience you can handle.
If you’re struggling and nothing else has worked, talk to a psychiatrist who specializes in treatment-resistant depression. Ask about both options. Don’t assume one is better just because it’s FDA-approved. The data doesn’t always back that up.
Depression doesn’t wait. And neither should you.
Is ketamine FDA-approved for depression?
Ketamine itself is not FDA-approved for depression. It was approved in 1970 as an anesthetic. Its use for depression is off-label, though widely supported by research. Esketamine, a component of ketamine, is FDA-approved as Spravato® for treatment-resistant depression.
How quickly do ketamine and esketamine work?
IV ketamine can reduce depression symptoms within hours-sometimes after the first treatment. Esketamine usually takes two doses before noticeable improvement. Both work far faster than traditional antidepressants, which can take 4-6 weeks.
Can I take ketamine or esketamine at home?
No. Both require administration under medical supervision. After receiving either, you must stay at the clinic for at least two hours for monitoring. You cannot drive yourself home. This is a safety requirement due to dissociative side effects.
Are ketamine and esketamine addictive?
Both are classified as Schedule III controlled substances, meaning they have potential for abuse but are considered medically useful. When used under professional supervision for depression, the risk of addiction is low. Misuse outside clinical settings, especially recreationally, carries higher risks.
Do I need to keep taking antidepressants while on ketamine or esketamine?
Yes. Both treatments are approved for use alongside an oral antidepressant. They’re not meant to replace your current medication-they’re meant to boost it. Stopping your antidepressant while using ketamine or esketamine can reduce long-term effectiveness.
How many treatments will I need?
For IV ketamine, most patients get 6-8 infusions over 2-4 weeks, then maintenance doses every 1-3 weeks. For esketamine, the FDA recommends twice weekly for 4 weeks, then once weekly for 4 weeks, then every 1-2 weeks as maintenance. Response varies, and dosing is personalized.
Will insurance cover ketamine or esketamine?
Esketamine (Spravato®) is covered by about 67% of commercial insurance plans. IV ketamine is covered by only 38% because it’s used off-label. Some clinics offer payment plans or sliding scales. Always check with your insurer and ask the clinic for a pre-authorization letter.
What are the long-term outcomes?
Studies show that about half of patients who respond to either treatment maintain improvement for six months with regular maintenance doses. IV ketamine has slightly higher remission rates at 6 months (56.3%) compared to esketamine (48.7%). Long-term data beyond one year is still limited.