Since 2018, a quiet but dangerous problem has been creeping into medicines millions of people rely on every day. It’s not about fake pills or expired stock. It’s about nitrosamine contamination in generic drugs - tiny, invisible chemical impurities that can increase cancer risk even at nanogram levels. What started with a single recall of valsartan has snowballed into a global crisis affecting hundreds of drug products, shaking trust in the generic drug system, and forcing manufacturers to rethink how medicines are made.
What Are Nitrosamines and Why Do They Matter?
Nitrosamines are a group of chemical compounds that form when certain amines react with nitrites under specific conditions. They’re not new - some are found in cured meats, tobacco smoke, and even beer. But when they show up in pills, the stakes change. The International Agency for Research on Cancer classifies several nitrosamines as probable or possible human carcinogens. That means even tiny amounts over long periods could raise cancer risk.
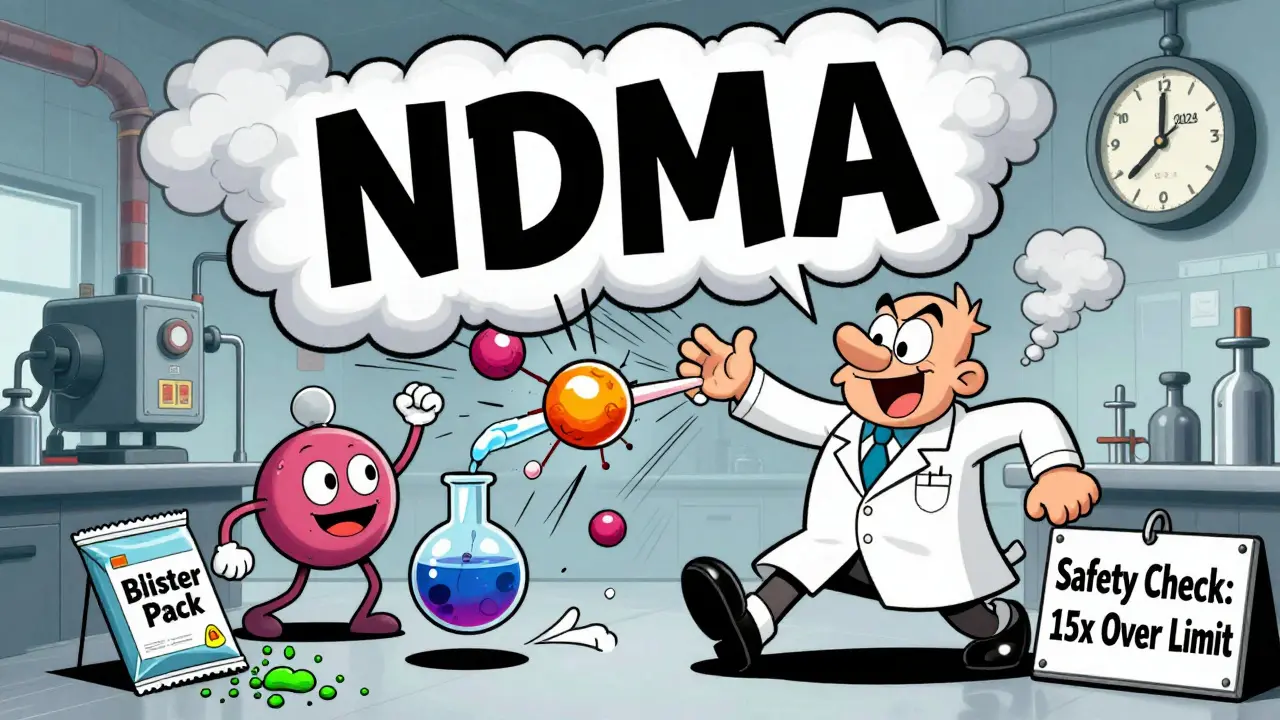
The FDA set strict limits based on lifetime exposure. For NDMA (N-Nitrosodimethylamine), the acceptable daily intake is 96 nanograms. For NDEA (N-Nitrosodiethylamine), it’s even lower: 26.5 nanograms. To put that in perspective, 96 nanograms is less than a grain of salt in a swimming pool. But in drug manufacturing, even that tiny amount can be too much if it’s not controlled.
The First Wave: Valsartan and the Domino Effect
The crisis exploded in 2018 when the FDA announced that valsartan, a common blood pressure medication, contained NDMA. The drug was made by a Chinese supplier whose manufacturing process accidentally created the impurity. Within weeks, recalls spread across multiple ARBs - losartan, irbesartan, olmesartan. Over 10 products vanished from U.S. shelves in just a few months.
But valsartan wasn’t the end. It was the start. By 2019, ranitidine (Zantac) was pulled after tests showed it could form NDMA inside the body. Then came metformin, the most widely prescribed diabetes drug. Then duloxetine, varenicline, and even antibiotics like rifampin. Each recall forced patients to switch medications, sometimes with no clear alternative. Pharmacies ran out of stock. Doctors scrambled. Patients worried.
How Do Nitrosamines Get Into Pills?
It’s not one mistake. It’s a chain of small oversights. The FDA found that nitrosamines form during manufacturing when secondary or tertiary amines react with nitrite impurities in solvents, reagents, or even excipients like magnesium stearate. One supplier’s batch of magnesium stearate contaminated three different ARB products - a single point of failure that rippled across multiple drugs.
But the biggest surprise came in 2022. Packaging materials were found to be culprits. Blister films, bottle liners, and even adhesives used in packaging contained secondary amines that reacted with nitrites over time. A 2024 case study showed an antibiotic tablet exceeded the safe limit not because of its ingredients, but because of the plastic blister pack it was stored in. Shelf life wasn’t just about stability - it was about chemical reactions happening inside the package.
Global Response: Who’s Doing What?
The FDA has led the charge. By mid-2025, it had overseen over 500 recalls tied to nitrosamines. It also published detailed guidance in September 2024, requiring manufacturers to test for over 20 specific nitrosamines, including drug substance-related impurities (NDSRIs) like N-nitroso-varenicline. Each has its own limit, and if multiple impurities are present, the total risk must not exceed 100%.
Other agencies followed, but slower. The EMA issued 32 recalls. Health Canada, the UK’s MHRA, and Japan’s PMDA each reported between 5 and 15. The FDA’s approach is more aggressive: it demands compound-specific limits, while the EMA allows broader thresholds. That’s why U.S. manufacturers face tougher testing and reformulation demands than their European counterparts.
The Human Cost: What It Takes to Fix This
Fixing nitrosamine contamination isn’t just about changing a filter. It’s about rebuilding entire processes. One mid-sized generic manufacturer spent 18 months and over $2 million just to fix its metformin line. They had to revalidate every step - from raw material sourcing to final packaging. They tested over 300 batches. They switched suppliers. They redesigned their drying process. All to reduce a contaminant that was present at 1,500 nanograms per day - 15 times the limit.
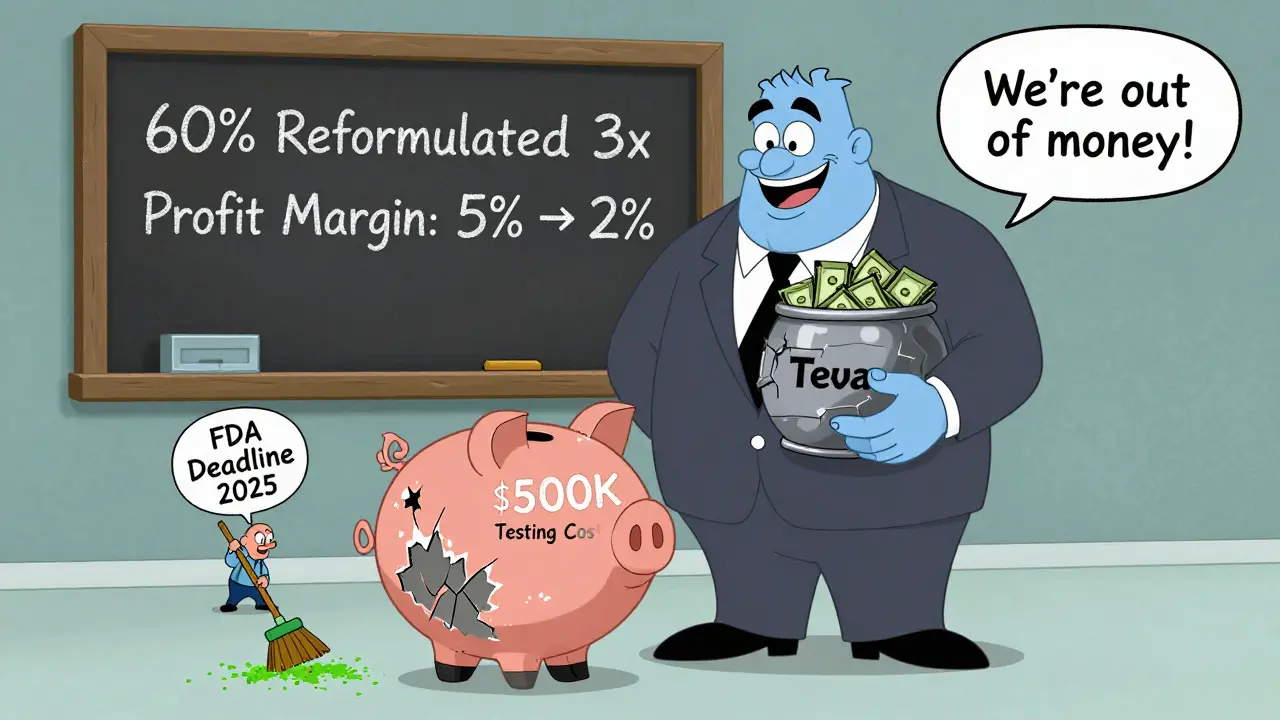
Another company found that fixing one pathway created another. They removed a nitrite-containing solvent, only to discover that a new excipient they switched to had trace amines. Then, the new packaging material introduced a third risk. It took three redesigns before they got it right. That’s not unusual. Industry reports show 60% of manufacturers had to go through multiple reformulation cycles.
Who’s Getting Hit the Hardest?
Small and mid-sized generic manufacturers are bearing the heaviest burden. Testing for nitrosamines requires expensive LC-MS/MS equipment. Training staff to interpret results takes months. The FDA estimates comprehensive testing programs cost $500,000 to $2 million per year for a typical generic maker. For a company with thin margins, that’s not just an expense - it’s a threat to survival.
Big players like Teva, Fresenius Kabi, and Sun Pharma have absorbed the costs. They have the labs, the teams, and the cash reserves. Smaller firms? Many are choosing to exit the market. Evaluate Pharma’s 2025 analysis found that nitrosamine compliance has cut generic drug profit margins by 3 to 5 percentage points. That’s enough to kill a business that already operates on 5% net margins.
The June 2025 Shift: FDA Relaxes the Deadline
In June 2025, the FDA made a major move. It had originally set August 1, 2025, as the deadline for full compliance with NDSRI controls. But in a rare acknowledgment of real-world challenges, it softened the rule. Now, manufacturers don’t need to be fully compliant by that date. Instead, they must submit progress reports in their annual filings, detailing what steps they’ve taken, what’s left, and when they expect to finish.
This wasn’t a surrender. It was a strategic pause. The FDA admitted that root cause investigations and stability data collection take longer than anyone expected. For a drug that’s been on the market for 20 years, proving that a reformulated version is just as stable over 36 months isn’t quick. The agency recognized that forcing deadlines without flexibility would cause more shortages than it prevented.
What’s Next?
The nitrosamine crisis isn’t over. It’s evolving. The FDA is now looking at other drug classes - including antivirals, antifungals, and even over-the-counter pain relievers. Analysts predict more recalls in 2026. The real question isn’t whether more drugs will be affected. It’s whether the system can adapt without breaking.
Manufacturers who acted early - testing during development, auditing suppliers, redesigning packaging - are now ahead. Those who waited are playing catch-up. And patients? They’re left wondering if the pills they take are safe. The answer isn’t simple. But the system is changing. Slowly. Carefully. And with more transparency than ever before.
Are all generic drugs unsafe because of nitrosamines?
No. Only a small fraction of generic drugs have been affected - and most of those have been recalled and replaced. The FDA and other regulators now require manufacturers to test for nitrosamines before products hit the market. If a drug is currently on the shelf and hasn’t been recalled, it’s been cleared for safety. Don’t stop taking your medication unless your doctor tells you to.
Can I test my medicine at home for nitrosamines?
No. Detecting nitrosamines requires lab equipment that can measure parts per billion - something like a gas chromatograph with mass spectrometry. You can’t buy this gear. Even if you could, interpreting the results requires expertise. If you’re concerned about your medication, check the FDA’s recall list or ask your pharmacist. Don’t try to test it yourself.
Why did it take so long for regulators to catch this?
Nitrosamines weren’t on anyone’s radar until 2018. The science to detect them at such low levels didn’t exist in most labs. Even when they were suspected, testing wasn’t required. Once valsartan was found to contain NDMA, regulators scrambled to build the tools and standards. It’s a classic case of a problem being invisible until a single example forces a system to wake up.
Is the FDA being too strict?
Some say yes. The limits are based on theoretical lifetime cancer risk, not proven cases in humans. But regulators err on the side of caution with carcinogens. A single nanogram might not hurt you - but if millions take a drug daily for years, even a tiny risk adds up. The FDA’s approach isn’t perfect, but it’s the most comprehensive in the world. And it’s saved lives.
What should I do if my generic drug was recalled?
Contact your pharmacist or doctor immediately. They’ll help you switch to a safe alternative - either a different generic or the brand-name version. Don’t stop taking your medication abruptly, especially for blood pressure or diabetes drugs. A sudden change can be dangerous. Your healthcare provider will guide you through a safe transition.