anti-IgA antibodies: What They Are, Why They Matter, and How They Affect Medication Safety
When your body makes anti-IgA antibodies, specialized immune proteins that target immunoglobulin A, a key antibody in mucosal defense. Also known as IgA-specific antibodies, they can cause severe reactions when someone with low or no IgA receives blood products, IVIG, or even some vaccines containing trace amounts of IgA. This isn’t just a rare lab curiosity—it’s a real risk in clinical settings, especially for people with selective IgA deficiency, which affects about 1 in 600 people.
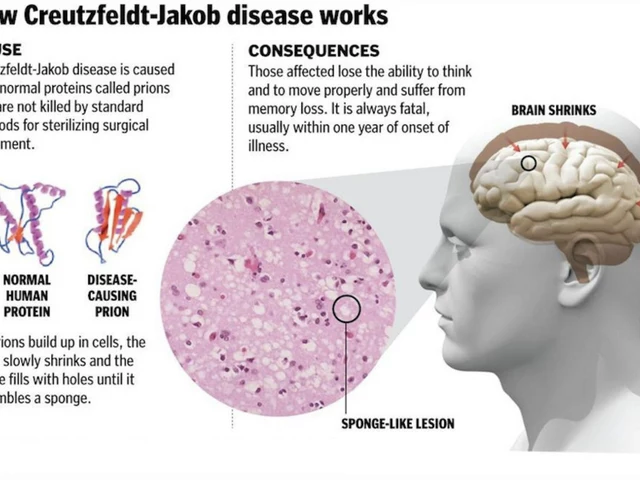
These antibodies don’t usually cause problems on their own. But when they meet IgA in a transfusion or injection, they can trigger anaphylaxis—sudden, life-threatening swelling, low blood pressure, and breathing trouble. That’s why hospitals screen high-risk patients before giving certain biologics. It’s also why some medications come with warnings about IgA content. The immunoglobulin A, the main antibody found in saliva, tears, and the gut lining is normally harmless. But in people who’ve never made it themselves, even tiny amounts from outside sources look like invaders.
Doctors don’t test everyone for anti-IgA antibodies. But if you’ve had a sudden allergic reaction during or right after a blood transfusion, IVIG, or even a vaccine, it’s worth asking. The same goes if you’ve been diagnosed with IgA deficiency and are starting a new treatment. Some drugs, especially those made from human plasma, carry a higher risk. Even though most modern products are purified to remove IgA, trace amounts can still slip through. That’s where pharmacovigilance, the science of monitoring drug safety and spotting unexpected reactions comes in—tracking these rare but dangerous events helps improve labeling and patient safety.
What you’ll find in the posts below isn’t just theory. These are real-world cases and practical insights: how drug safety alerts flag IgA-related risks, why some people react to medications others tolerate fine, and how doctors use dechallenge and rechallenge to confirm if a reaction was truly caused by a drug. You’ll see how batch variability in biologics can affect IgA content, how medication adherence matters when you’re on a risky treatment, and why knowing your own immune history can prevent hospital visits. This isn’t about memorizing terms—it’s about understanding what your body might be reacting to, and how to speak up before it turns dangerous.