CSM: Understanding Drug Safety, Adverse Reactions, and Patient-Centered Care
When we talk about CSM, a framework used in pharmacovigilance to classify and respond to drug safety concerns. Also known as Clinical Safety Monitoring, it’s not just a checklist—it’s the system that helps doctors and patients catch dangerous drug reactions before they turn into emergencies. CSM is what ties together everything from a patient’s missed pill to a life-threatening interaction between two common medications. It’s why we track side effects, why pharmacies warn about alcohol with certain drugs, and why your doctor asks if you’ve had any strange symptoms since starting a new medicine.
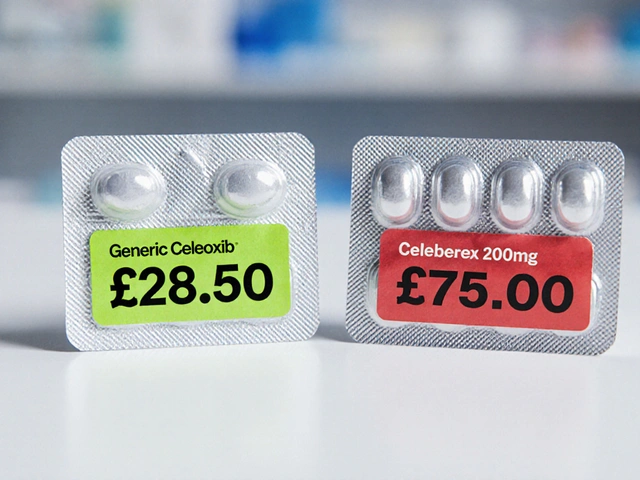
CSM doesn’t work in isolation. It connects directly to adverse drug reactions, unintended and harmful responses to medications at normal doses. This includes everything from mild rashes to fatal heart rhythms. The same system that flags a drug-specific warning for a new antibiotic also explains why some people get severe yeast infections from diabetes drugs like SGLT2 inhibitors. It’s how we know that stopping a drug (dechallenge) and restarting it (rechallenge) can prove whether a side effect is real—or just a coincidence. And it’s why batch variability in generics matters: if two pills from different batches behave differently in your body, CSM is the process that catches it. CSM also links to pharmacovigilance, the science of detecting, assessing, and preventing adverse effects of medicines. This isn’t just FDA paperwork—it’s real-time monitoring by doctors, pharmacists, and patients who report weird symptoms. That’s how we learned that antihistamines can trigger delirium in older adults, or that certain psychiatric combos can cause serotonin syndrome. CSM turns patient stories into safety rules. And it’s why medication adherence, how consistently a patient takes their medicine as prescribed—is part of the equation. If someone skips doses, the drug’s effect changes. That’s not noncompliance—it’s a signal. CSM helps us ask: Is the side effect worse because they took too much? Or because they didn’t take enough?
What you’ll find here isn’t theory. These are real cases: a man who nearly died from a transfusion because no one checked for IgA deficiency. A child who finally took their antibiotic after it was flavored. An elderly woman whose confusion cleared up the day her anticholinergic was stopped. These aren’t anomalies—they’re patterns CSM was built to uncover. Whether you’re managing your own meds, caring for someone with multiple prescriptions, or just trying to understand why a drug you trust suddenly has a warning label, this collection gives you the tools to ask the right questions. No jargon. No fluff. Just what you need to stay safe and in control.