Delirium Prevention: How to Reduce Risk and Protect Brain Health
When someone suddenly becomes confused, agitated, or unaware of where they are, it’s often not dementia—it’s delirium, a sudden, temporary state of confusion caused by physical or mental stress on the brain. Also known as acute confusional state, it’s not a disease but a warning sign that something serious is happening inside the body. Unlike dementia, which slowly worsens over years, delirium can appear in hours or days—and it’s often preventable.
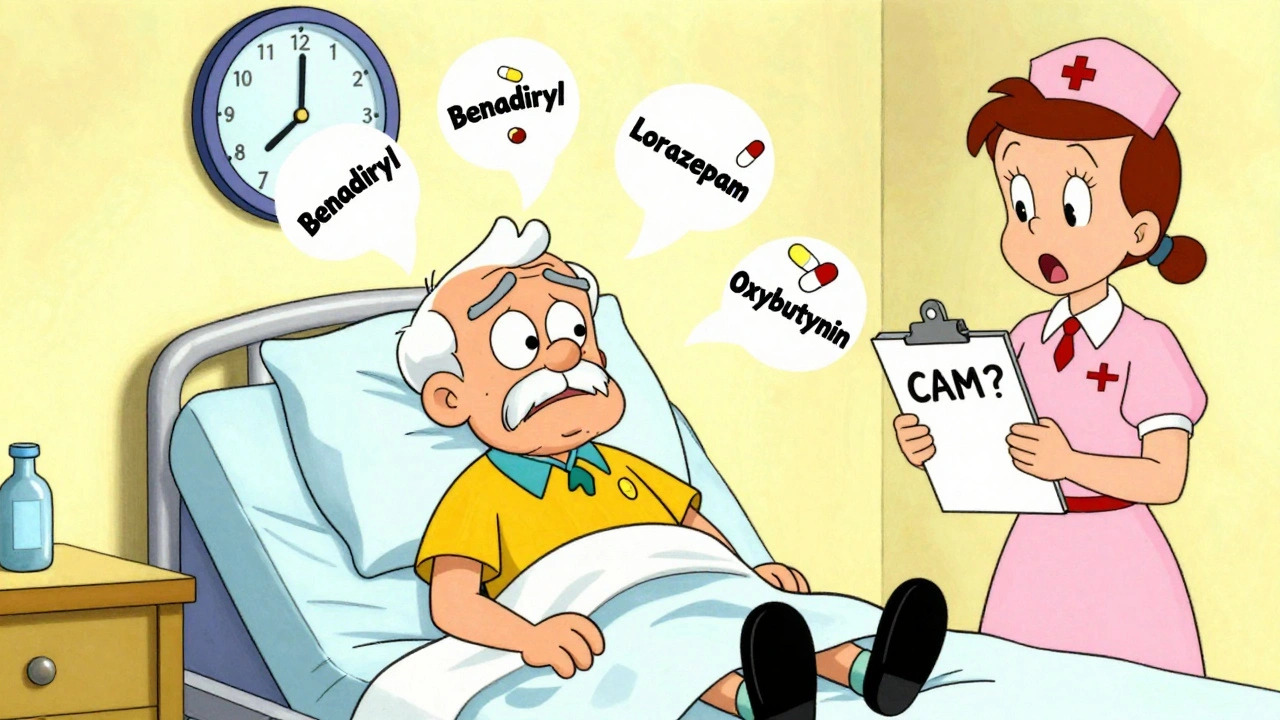
Delirium most commonly strikes older adults, especially those in hospitals or nursing homes, but it can happen to anyone after surgery, infection, or even a bad reaction to medication. Medication safety, the careful use and monitoring of drugs to avoid brain-altering side effects is one of the biggest levers for prevention. Many common drugs—sleep aids, painkillers, antihistamines, even some heart meds—can trigger delirium in vulnerable people. The same pill that helps one person sleep might send another into confusion. That’s why knowing your meds and asking about side effects isn’t optional—it’s critical.
It’s not just drugs. Delirium risk factors, conditions or situations that increase the chance of sudden confusion include dehydration, sleep disruption, untreated pain, and sensory overload. A noisy ICU room, no glasses or hearing aids, being tied to a bed, or not knowing the time of day can all pile up and push someone over the edge. Simple fixes—like keeping the room quiet, ensuring glasses are on, letting someone know the date and time, or getting them out of bed to sit in a chair—can make a huge difference.
Family members and caregivers play a huge role. If you notice a loved one acting strangely—forgetting names, talking nonsense, staring blankly, or suddenly sleepy—you can’t wait to see if it gets better. Call the doctor immediately. Early intervention can stop delirium from turning into longer-term cognitive decline. Studies show that people who experience delirium are far more likely to develop lasting memory problems or need long-term care later on. That’s why prevention isn’t just about comfort—it’s about protecting someone’s future independence.
There’s no magic pill for delirium prevention, but there are proven habits. Keep hydration high. Avoid unnecessary meds. Maintain routines. Get sunlight and movement. Monitor for infections—especially urinary or lung infections, which are silent triggers. And if you’re in the hospital, ask: "Is this drug really needed?" and "Can we check for delirium today?" These questions save brain function.
Below, you’ll find real-world stories and science-backed tips on how to spot early signs, reduce medication risks, and create safer environments for those most vulnerable. These aren’t abstract ideas—they’re actions that families and caregivers use every day to keep people sharp, safe, and present.