Managing Opioid Symptoms: Signs, Risks, and Practical Steps
When you're managing opioid symptoms, the physical and emotional effects that come from using or stopping opioid medications. Also known as opioid withdrawal management, it's not just about stopping pain—it's about staying safe, avoiding relapse, and rebuilding control over your body. Opioids, whether prescribed for pain or used differently, change how your brain and nervous system work. When you reduce or stop them, your body reacts. That’s when symptoms like nausea, sweating, anxiety, muscle aches, and insomnia show up. These aren’t just uncomfortable—they can be dangerous if handled alone.
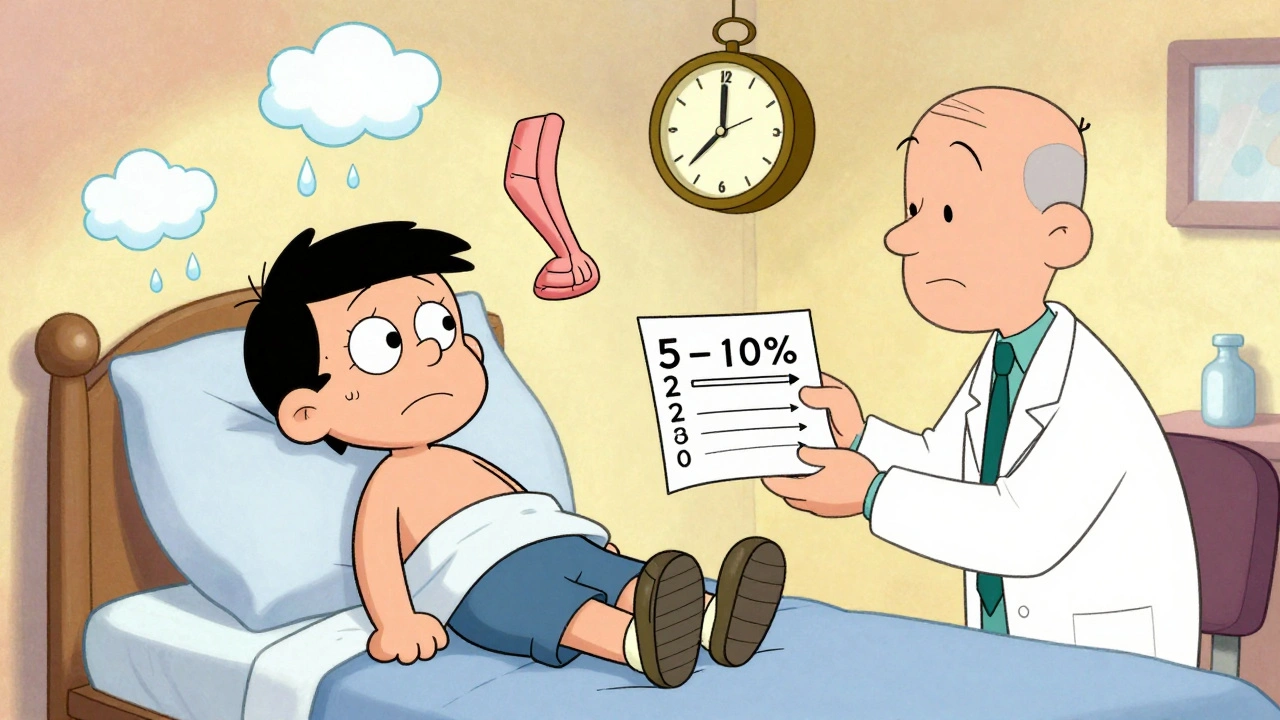
One key thing to know: opioid withdrawal, the set of physical and psychological symptoms that occur when opioid use is reduced or stopped. Also known as opioid discontinuation syndrome, it typically starts within hours and peaks in 2–3 days. But it’s not the only concern. Long-term use leads to opioid dependence, a condition where the body relies on the drug to function normally. Also known as physical opioid tolerance, it means you need more of the drug to get the same effect—and stopping feels impossible without help. Many people confuse dependence with addiction, but they’re different. Dependence is physical. Addiction includes compulsive use despite harm. Both need support, but the approach changes.
Side effects like constipation, drowsiness, and slowed breathing aren’t just annoyances—they’re warning signs. If you’re on long-term opioids, your doctor should monitor your breathing, liver function, and mental health. Tools like medication logs and adherence checklists help track patterns. And if you’re switching or stopping, don’t go cold turkey. Tapering under medical supervision cuts risks by more than half. Even small steps—like staying hydrated, using heat packs for muscle pain, or getting light exercise—can make withdrawal more manageable.
There’s no one-size-fits-all fix. What works for someone on prescription oxycodone might not help someone who’s been using heroin. That’s why the best advice comes from real experiences: tracking symptoms, knowing your limits, and asking for help early. The posts below cover what actually works—from spotting early signs of overdose to understanding how long symptoms last, how to talk to your doctor about reducing doses, and what alternatives exist for chronic pain. You’ll find clear, no-fluff guidance from people who’ve been there—and the science behind what helps.