PDC Score: What It Is and How It Affects Medication Safety
When doctors prescribe a drug, they expect it to work—but it only works if you take it right. That’s where the PDC score, a metric that measures the proportion of days a patient has the prescribed medication available over a given period. Also known as proportion of days covered, it’s not just a number—it’s a real-world indicator of whether your treatment plan is actually helping you. A PDC score of 80% or higher is generally considered good for chronic conditions like high blood pressure or diabetes. But if your score drops below that, your risk of hospitalization, complications, or even death goes up—no matter how good the drug is.
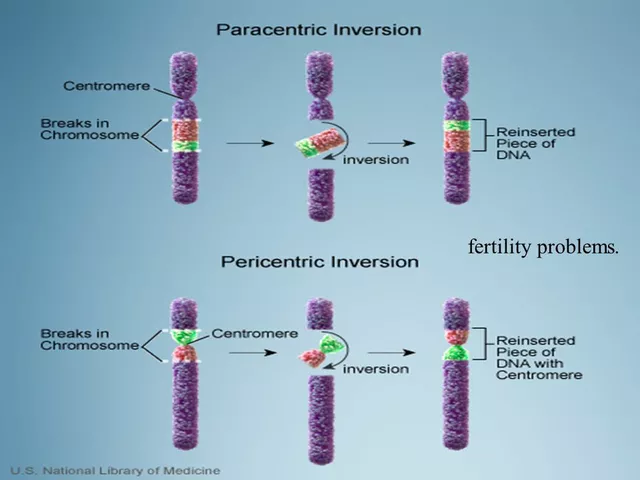
The PDC score doesn’t care if you meant to take your pills. It only tracks whether you had them in hand when you needed them. That’s why it’s closely tied to medication adherence, the extent to which a patient follows their prescribed treatment plan. It’s also deeply connected to pharmacodynamics, how a drug affects the body over time. If you skip doses, the drug’s effect fades. If you take too much, side effects pile up. And if you stop cold turkey—like with opioids or antidepressants—you risk withdrawal or relapse. That’s why posts on this page cover everything from how flavoring kids’ meds boosts adherence, to why step therapy makes people quit their prescriptions, to how batch variability in generics can make you miss doses because the pill looks different.
What’s surprising is how often the PDC score fails silently. A patient might have a perfect prescription, but if they can’t afford it, don’t understand it, or get confused by too many pills, the score plummets. That’s why medication lists for caregivers, prior authorization appeals, and even prescription writing errors all tie back to this one number. Even something as simple as a pill’s size or taste can drop your PDC score. And when it does, your body pays the price—in flare-ups, infections, or hospital visits.
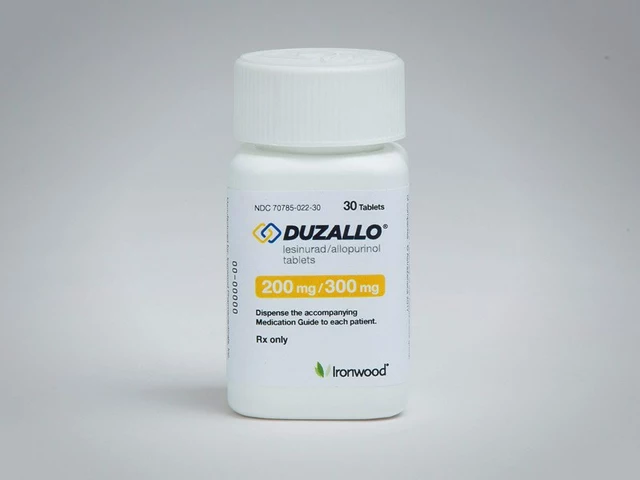
On this page, you’ll find real stories and data about what actually happens when people don’t take their meds right. From how SGLT2 inhibitors cause yeast infections because patients stop them when they feel weird, to how antipsychotics lead to weight gain because people skip doses to avoid side effects, the pattern is clear: adherence isn’t about willpower—it’s about design, access, and understanding. The posts here don’t just explain the problem. They show you how to fix it—at the pharmacy, at home, and in the clinic.